Identifying Family Support Mechanisms in Postpartum Psychological Adjustment
Keywords:
postpartum psychological adjustment, family support, emotional well-being, qualitative research, maternal mental healthAbstract
Objective: This study aimed to explore the mechanisms through which family support contributes to the psychological adjustment of postpartum women.
Methods and Materials: A qualitative research design was employed using semi-structured interviews with 23 postpartum women residing in Bangladesh. Participants were recruited through purposive sampling and represented a range of ages, educational backgrounds, and parity statuses. Data collection continued until theoretical saturation was reached. All interviews were transcribed verbatim and analyzed using thematic analysis, following Braun and Clarke’s six-step framework. NVivo 14 software facilitated systematic coding and theme development. Ethical approval was obtained, and all participants gave informed consent.
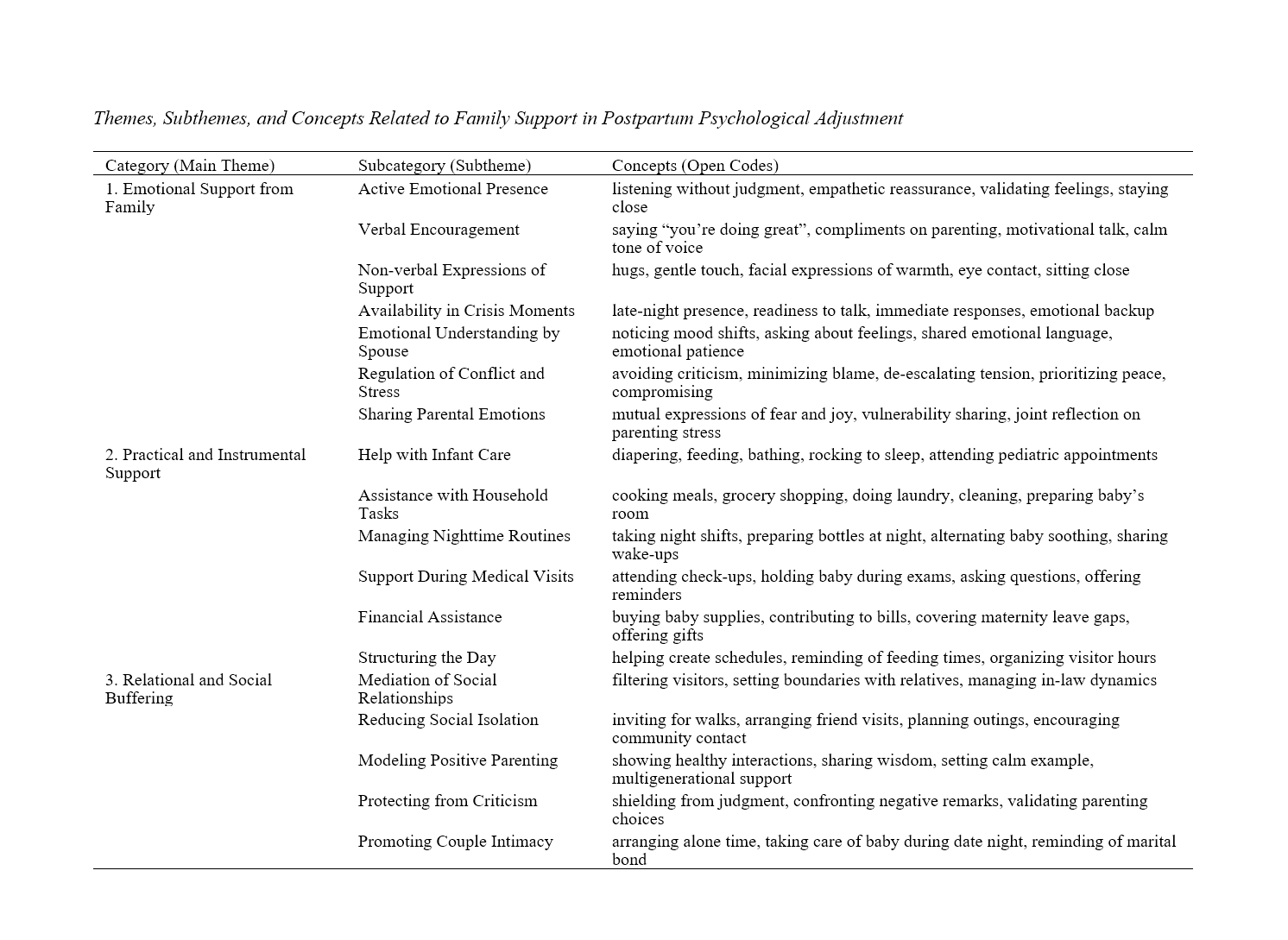
Findings: Three main themes emerged: (1) Emotional Support from Family (including subthemes such as active emotional presence, verbal encouragement, and emotional understanding from the spouse), (2) Practical and Instrumental Support (including help with infant care, household tasks, and medical visits), and (3) Relational and Social Buffering (including protection from criticism, mediation of social relations, and promotion of couple intimacy). Across all themes, the perceived quality and timing of support were central to their psychological impact. Participants who experienced emotionally attuned, respectful, and reliable support reported greater psychological stability, reduced distress, and enhanced postpartum coping.
Conclusion: The findings underscore that family support in the postpartum period is not solely about the presence of assistance but is critically shaped by its relational quality, emotional sensitivity, and alignment with maternal needs. Emotional reassurance, practical help, and protection from social stressors—when delivered with empathy and respect—can significantly buffer against psychological distress and promote adjustment. These insights suggest a need for culturally sensitive, family-inclusive mental health interventions tailored to postpartum women.
Downloads
References
Dağ, İ., & Değer, V. B. (2025). The Importance of Psychological Well-Being for Women: Ways to Cope With Stress and Postnatal Depression. https://doi.org/10.5772/intechopen.1009206
Eitenmüller, P., Köhler, S., Hirsch, O., & Christiansen, H. (2022). The Impact of Prepartum Depression and Birth Experience on Postpartum Mother-Infant Bonding: A Longitudinal Path Analysis. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.815822
Feldman, N., & Perret, S. (2023). Digital Mental Health for Postpartum Women: Perils, Pitfalls, and Promise. NPJ Digital Medicine, 6(1). https://doi.org/10.1038/s41746-023-00756-4
Fitriana, F., Ningtyas, W. S., & Dewi, E. R. (2022). Providing Mental Healthcare for Postpartum Women in Indonesia: A Qualitative Phenomenological Study. British Journal of Midwifery, 30(12), 692-699. https://doi.org/10.12968/bjom.2022.30.12.692
Goldberg, A. E., & Frost, R. L. (2024). “Saying ‘I'm Not Okay’ Is Extremely Risky”: Postpartum Mental Health, Delayed Help‐seeking, and Fears of the Child Welfare System Among Queer Parents. Family Process, 64(1). https://doi.org/10.1111/famp.13032
Hanson, M. N., Reese, S. E., & Newcomer, S. R. (2023). Challenges in Accessing Mental Health Care During Pregnancy and Postpartum in Rural Montana. MCN the American Journal of Maternal/Child Nursing, 48(5), 252-257. https://doi.org/10.1097/nmc.0000000000000937
Iyengar, U., & Hunt, J. M. (2024). An Open Conversation About Postpartum PsychosisAn Interview With Jessie Hunt: Communications Lead, Advocate, and Expert By Experience. The Yale Journal of Biology and Medicine, 97(1), 107-112. https://doi.org/10.59249/pwxz3821
Kahaki, F. (2024). The Role of Social Support Systems in Enhancing Mental Health in Women Experiencing Postpartum Depression. PWJ, 5(4), 111-119. https://doi.org/10.61838/kman.pwj.5.4.13
M.Y, Y. S., Samsinar, S., & Intani, T. M. (2025). The Influence of Social Support on Postpartum Depression Risk Among Pregnant Women. Thejoas, 2(2), 587-595. https://doi.org/10.59613/qkhvsw65
Modak, A., Ronghe, V., Gomase, K., Mahakalkar, M., & Taksande, V. (2023). A Comprehensive Review of Motherhood and Mental Health: Postpartum Mood Disorders in Focus. Cureus. https://doi.org/10.7759/cureus.46209
Mousa, O., Sabati, S. Y. A., & Khars, F. A. (2023). Postpartum Depression: Neglected Issue in Maternal Health. International Journal of Nursing Education, 15(1), 72-77. https://doi.org/10.37506/ijone.v15i1.18995
Muliyani, N., & Suryaningsih, E. K. (2023). The Effect of Family Support on Postpartum Depression : Scoping Review. Indigenous Jurnal Ilmiah Psikologi, 8(3), 337-351. https://doi.org/10.23917/indigenous.v8i3.2165
Narumoto, K., Endo, M., Kaneko, M., Iwata, T., & Inoue, M. (2024). Japanese Primary Care Physicians' Postpartum Mental Health Care: A Cross‐sectional Study. Journal of General and Family Medicine, 25(4), 224-231. https://doi.org/10.1002/jgf2.700
Ojomo, O., Alesinloye-King, O., Erlandsson, K., Ängeby, K., & Envall, N. (2023). Mental Health Conditions in the Postpartum Period: A Scoping Study. https://doi.org/10.21203/rs.3.rs-2623747/v1
Putri, A. S., Wurisastuti, T., Suryaputri, I. Y., & Mubasyiroh, R. (2023). Postpartum Depression in Young Mothers in Urban and Rural Indonesia. Journal of Preventive Medicine and Public Health, 56(3), 272-281. https://doi.org/10.3961/jpmph.22.534
Rawal, S. (2025). Mental Health Awareness and Access to Services in Postpartum Women. Journal of Pharmacy and Bioallied Sciences, 17(Suppl 1), S417-S419. https://doi.org/10.4103/jpbs.jpbs_1593_24
Sagala, H. (2023). The Role of Midwives in Recognizing Signs and Symptoms of Postpartum Depression. Journal of Psychiatry Psychology and Behavioral Research, 4(1), 20-21. https://doi.org/10.21776/ub.jppbr.2023.004.01.6
Sarantaki, A., & Vivilaki, V. (2021). Postpartum Depression in Women Refugees/Asylum Seekers- Recognition and Coping Strategies. International Journal of Psychiatry Research, 4(5). https://doi.org/10.33425/2641-4317.1107
Upalkar, Y. (2025). Prevalence and Correlates of Postpartum Depression (PPD) in India: Literature Review-Based Study. Journal of Neonatal Surgery, 14(5S), 81-85. https://doi.org/10.52783/jns.v14.1988
Vidal, C. C., Marques, A. L. M., Jucá, A. L., Silva, E. V. d., Sandy de Oliveira Lemos, G., Cínthia Kalyne de Almeida, A., & Falcão, I. V. (2023). Occupational Therapy Practice With Puerperal Women in the Actions of the Family Health Support Center. Cadernos Brasileiros De Terapia Ocupacional, 31. https://doi.org/10.1590/2526-8910.ctoao268935042
Wu, Q., Radey, M., Han, S. J., Jalapa, K., Tawfiq, D., & McWey, L. M. (2023). Profiles of Perceived Resources Among Low‐income, Rural Mothers: Prospective Associations With Maternal and Child Outcomes. Family Process, 63(1), 331-347. https://doi.org/10.1111/famp.12862
Zakiyah, Z., Fitria, I., Wahyuni, S., Sipasulta, G. C., & Muna, S. (2025). Postpartum Maternal Mental Health: Identification of Risk Factors and Holistic Intervention Approaches. M.Journal, 2(2), 28-33. https://doi.org/10.69855/mgj.v2i2.122
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.