Ranking Determinants of Therapy Dropout Among Women
Keywords:
Therapy dropout, Women’s mental health, Therapeutic relationship, Treatment adherenceAbstract
Objective: This study aimed to identify and rank the primary determinants contributing to therapy dropout among women through an integrated mixed-method approach, highlighting the personal, relational, and systemic factors influencing discontinuation of psychological treatment.
Methods and Materials: A sequential exploratory mixed-method design was employed. In the qualitative phase, an extensive literature review was conducted until theoretical saturation was achieved, and data were analyzed using NVivo 14 to extract thematic categories and conceptual patterns. Seven main themes were identified, encompassing individual, cultural, and institutional determinants. In the quantitative phase, a structured questionnaire based on qualitative results was administered to 260 Chinese women who had prematurely discontinued therapy. Participants rated the importance of each determinant on a five-point Likert scale. Data were analyzed using SPSS 26, employing descriptive statistics, Cronbach’s alpha for reliability, and Kendall’s coefficient of concordance to assess consensus in ranking.
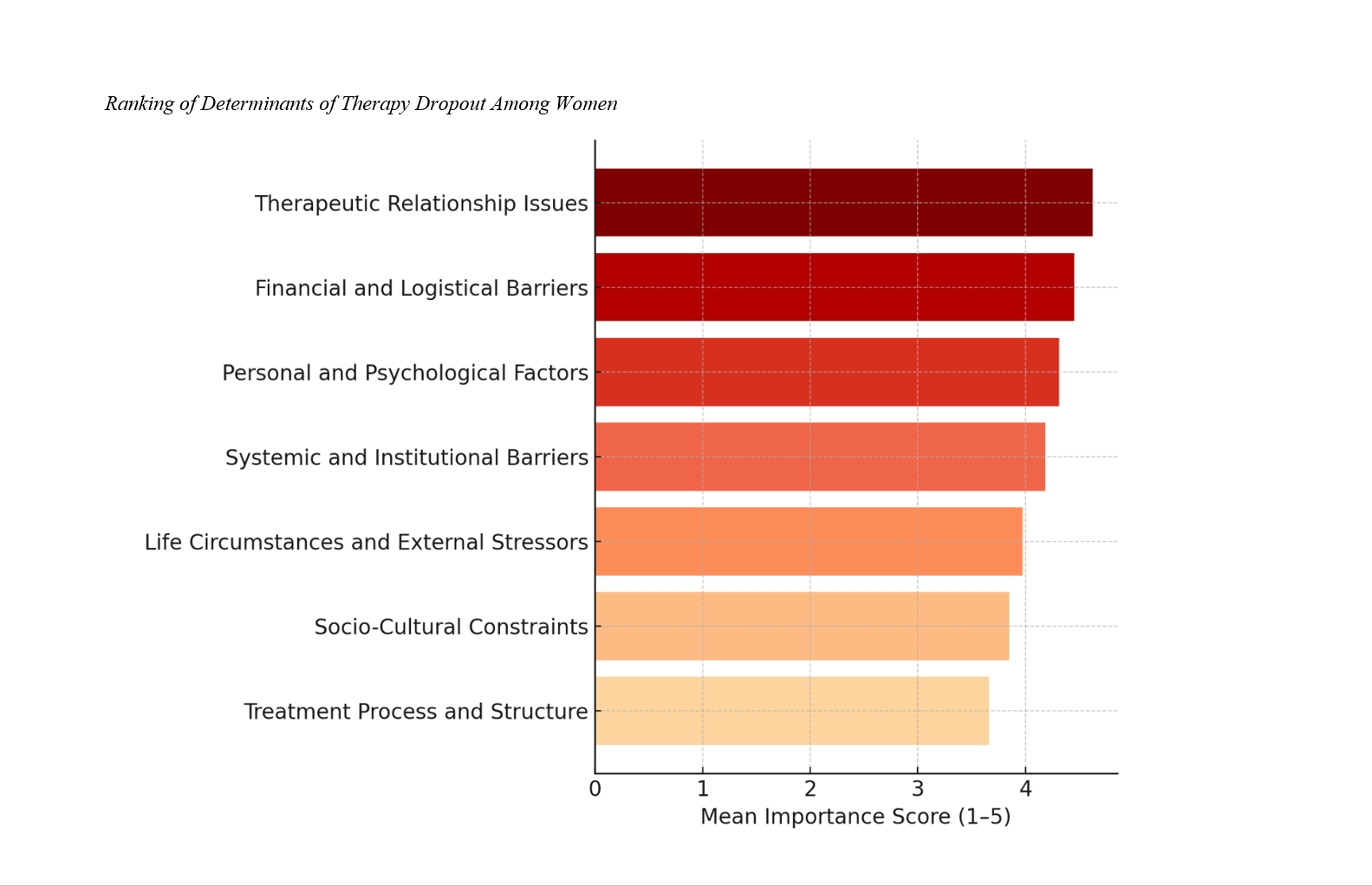
Findings: Results revealed that therapeutic relationship issues ranked as the most influential determinant (Mean = 4.62), followed by financial and logistical barriers (Mean = 4.45) and personal and psychological factors (Mean = 4.31). Systemic and institutional barriers (Mean = 4.18) and life circumstances and external stressors (Mean = 3.97) were moderately ranked, while socio-cultural constraints (Mean = 3.85) and treatment process and structure (Mean = 3.66) were identified as less decisive factors. Kendall’s W indicated a high level of agreement among participants, confirming the robustness of rankings.
Conclusion: Therapy dropout among women is shaped by intertwined relational, psychological, and structural determinants, with the therapeutic relationship emerging as the most critical factor. Enhancing empathy, cultural sensitivity, financial accessibility, and flexible service design is essential to reduce attrition and promote sustained engagement in therapy.
Downloads
References
Bakay, H., Karaağaç, M., Yaman, N. O., & Gıca, Ş. (2025). Verbal Mental Capacity and Medication Adherence in Psychiatric Outpatients: The Impact of Verbal Cognitive Reserve and Side Effects. Neuropsychiatric Investigation, 63(1), 1-7. https://doi.org/10.5152/neuropsychiatricinvest.2025.25045
Boakye, D. S., Setordzi, M., Dzansi, G., & Adjorlolo, S. (2024). Mental Health Burden Among Females Living With HIV and AIDS in Sub-Saharan Africa: A Systematic Review. Plos Global Public Health, 4(2), e0002767. https://doi.org/10.1371/journal.pgph.0002767
Changchien, T.-C., Hsieh, T.-J., & Yen, Y. C. (2024). Erectile Dysfunction Among Male Patients Receiving Methadone Maintenance Treatment: Focusing on Anxiety-Related Symptoms. Sexual Medicine, 12(4). https://doi.org/10.1093/sexmed/qfae052
Dhaliwal, J. S., Chan, L. G., Goh, J., Koh, K. H. E., & Wong, C. S. (2021). Mental Health and Implications for Antiretroviral Adherence in a Multiethnic Asian Cohort. Sexually Transmitted Infections, 98(7), 497-502. https://doi.org/10.1136/sextrans-2021-055153
Esfandiari, N., Mazaheri, M. A., Sadeghi‐Firoozabadi, V., & Cheraghi, M. (2020). Internet-Delivered vs Face-to-Face Cognitive Behavior Therapy for Anxiety Disorders: Systematic Review and Meta-Analysis (Preprint). https://doi.org/10.2196/preprints.18275
Ghafoori, B., Matos, M., & Gonçalves, M. (2022). Dropout From Evidence‐based Trauma Treatment in a Community Mental Health Clinic Serving Victims of Interpersonal Violence. Journal of Traumatic Stress, 35(3), 1025-1041. https://doi.org/10.1002/jts.22811
Kazemi, F., Omidi, F., Shahmoradi, Z., Ranjbaran, F., & Tajerian, A. (2024). Internalized Stigma and Adherence to Treatment Among Outpatients With Mental Illness. Iranian journal of psychiatry and behavioral sciences, 18(1). https://doi.org/10.5812/ijpbs-139384
Krendl, A. C., & Lorenzo‐Luaces, L. (2022). Identifying Peaks in Attrition After Clients Initiate Mental Health Treatment in a University Training Clinic. Psychological Services, 19(3), 519-526. https://doi.org/10.1037/ser0000469
Lakin, D. P., Win, K. S., Aung, H., Soe, K. N. C., Kyi, B., Marcell, A. V., Tol, W. A., & Bass, J. (2020). Masculinity and Mental Health Treatment Initiation for Former Political Prisoners in Yangon, Myanmar – A Qualitative Investigation. https://doi.org/10.21203/rs.3.rs-18159/v3
Lyles-Mckelvy, S., Wiafe, A., Zhang, X., Gupta, M. D., Hanna, M., Lee, H., Mejia, R., & Morton, K. R. (2024). Examining Social Determinates of Health in Adult Sickle Cell Disease Patients. Blood, 144(Supplement 1), 7678-7678. https://doi.org/10.1182/blood-2024-211727
Milanak, M. E., Witcraft, S. M., Park, J. Y., Hassell, K., McMahon, T., & Wilkerson, A. K. (2023). A Transdiagnostic Group Therapy for Sleep and Anxiety Among Adults With Substance Use Disorders: Protocol and Pilot Investigation. Frontiers in Psychiatry, 14. https://doi.org/10.3389/fpsyt.2023.1160001
Morcillo-Muñoz, Y., Sánchez-Guarnido, A. J., Calzón-Fernández, S., & Baena-Parejo, I. (2022). Multimodal Chronic Pain Therapy for Adults via Smartphone: Randomized Controlled Clinical Trial (Preprint). https://doi.org/10.2196/preprints.36114
Shafierizi, S., Basirat, Z., Nasiri‐Amiri, F., Kheirkhah, F., Geraili, Z., Pasha, H., & Faramarzi, M. (2024). Predictors of Nonresponse to Treatment and Low Adherence to Internet-Based Cognitive Behavioral Therapy in Depressed/Anxious Women Facing the Couple’s Fertility Problems: A Secondary Analysis of a Randomized Control Trial. BMC psychiatry, 24(1). https://doi.org/10.1186/s12888-023-05484-3
Thomas, M., Bramoweth, A. D., Seo, Y. J., Buysse, D. J., & Soreca, I. (2025). Evaluating Participation in Cognitive-Behavioral Therapy for Insomnia in Veterans Using Electronic Health Records. Sleep, 48(Supplement_1), A256-A256. https://doi.org/10.1093/sleep/zsaf090.0587