Ranking Lived Barriers to ADHD Diagnosis in Adult Women
Keywords:
ADHD, adult women, diagnostic barriers, gender bias, sociocultural stigma, emotional maskingAbstract
Objective: This study aimed to identify, categorize, and rank the lived barriers that adult women experience in obtaining an accurate and timely diagnosis of Attention-Deficit/Hyperactivity Disorder (ADHD) through an integrated mixed-method approach.
Methods and Materials: A sequential mixed-method design was employed, consisting of an initial qualitative phase followed by a quantitative ranking phase. In the qualitative phase, a systematic literature review was conducted until theoretical saturation, identifying six major thematic categories of diagnostic barriers using NVivo 14 software. These categories encompassed gendered diagnostic bias, emotional and psychological masking, sociocultural stigma and norms, systemic and institutional barriers, self-perception and help-seeking attitudes, and life-stage-specific challenges. In the quantitative phase, a structured questionnaire derived from the qualitative themes was administered to 225 adult women aged 20–55 years residing in Mexico. Participants rated each barrier on a five-point Likert scale. Descriptive and inferential analyses were conducted using SPSS version 26, including calculation of mean scores and Kendall’s W coefficient to assess agreement.
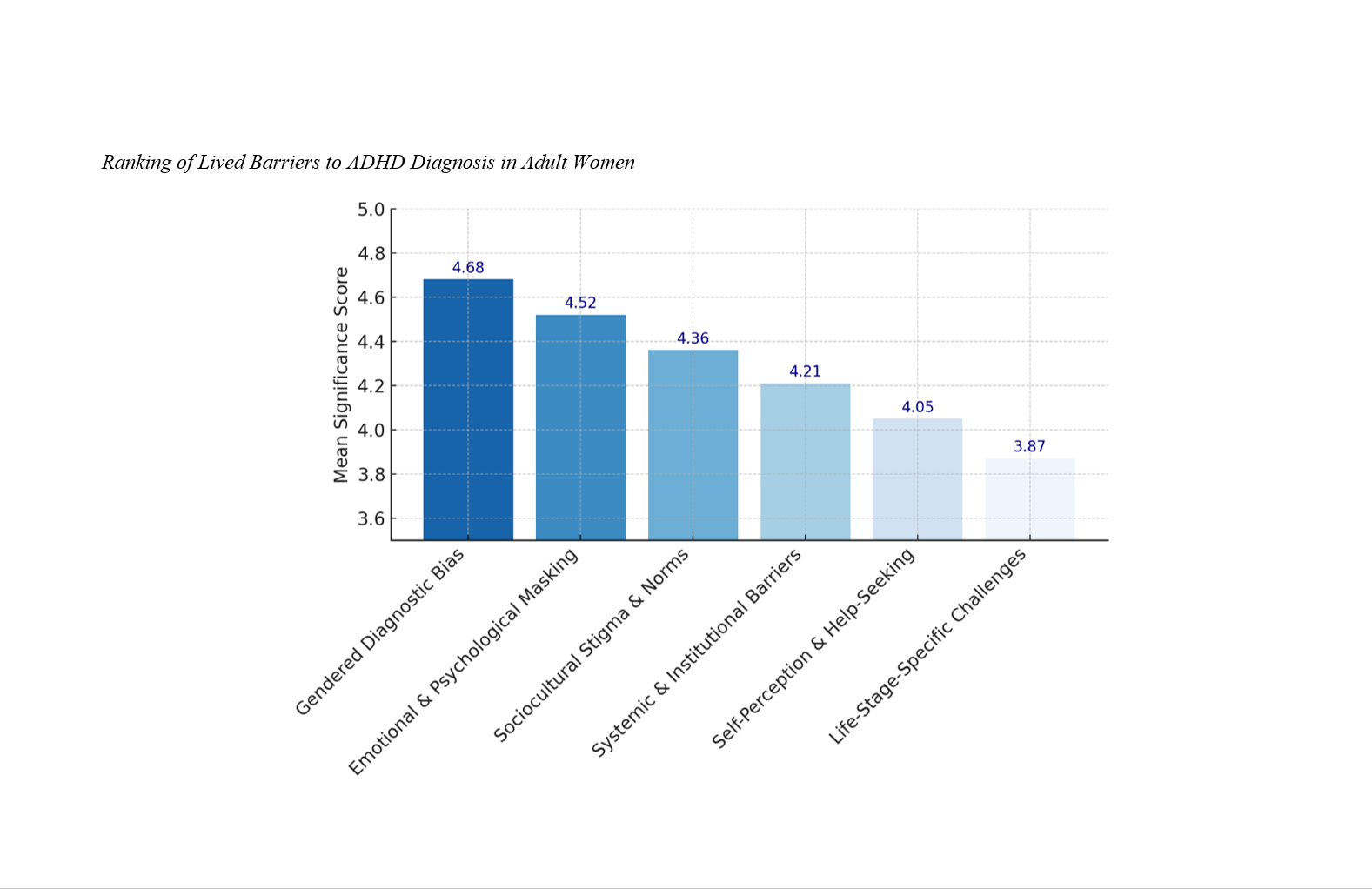
Findings: Results revealed strong concordance among participants regarding the hierarchy of barriers (Kendall’s W = 0.81, p < 0.001). Gendered diagnostic bias ranked as the most significant barrier (M = 4.68, SD = 0.41), followed by emotional and psychological masking (M = 4.52, SD = 0.47) and sociocultural stigma and norms (M = 4.36, SD = 0.56). Systemic and institutional barriers (M = 4.21, SD = 0.63), self-perception and help-seeking attitudes (M = 4.05, SD = 0.59), and life-stage-specific challenges (M = 3.87, SD = 0.68) followed in descending order.
Conclusion: The findings underscore the multidimensional nature of ADHD diagnostic inequities among adult women, revealing the interplay between clinical bias, cultural stigma, emotional masking, and systemic limitations.
Downloads
References
Bâ, S. A., Diop, E. D., Ngom, M., Diallo, B., Sene, E. G., Seck, P. A., & Dieng, A. (2025). Clinical Reflection Through Her Child: Presentation of a Case of Attention Deficit Disorder in Adulthood in a 35-Year-Old Woman. Saudi Journal of Medical and Pharmaceutical Sciences, 11(09), 902-906. https://doi.org/10.36348/sjmps.2025.v11i09.014
Bradley, S., Parzych, I., Platts, J., & Powell, L. (2025). Understanding and Harnessing Differences in Women With ADHD: A Qualitative Study. Neurodiversity, 3. https://doi.org/10.1177/27546330251317199
Budman, J., Maeir, A., Velder-Shukrun, I., & Zaguri‐Vittenberg, S. (2025). Effectiveness of the Cognitive–Functional Intervention for Adults (Cog–Fun A) in Assessing ADHD: A Retrospective Case Series. American Journal of Occupational Therapy, 79(4). https://doi.org/10.5014/ajot.2025.051045
Cameira, M., Abreu, P. E. d., Pereira, M. F. C., Soares, M., Vidó, I., Iza Paula de Carvalho, L., & Ramalheira, F. (2025). Navigating the Hormonal Labyrinth: Understanding the Impact of Menstrual Cycle Dynamics on ADHD Symptoms. European Psychiatry, 68(S1), S1186-S1186. https://doi.org/10.1192/j.eurpsy.2025.2398
Cıvan, H. Y., & Berkol, T. D. (2025). ADHD Comorbidity in Women With Depression and Anxiety: Prevalence, Clinical Features and Hyperfocus Dynamics. The International Journal of Psychiatry in Medicine. https://doi.org/10.1177/00912174251376111
Coll‐Martín, T., Carretero‐Dios, H., & Lupiáñez, J. (2024). Attention-Deficit/Hyperactivity Disorder Symptoms as a Function of Arousal and Executive Vigilance: Testing Halperin and Schulz’s Neurodevelopmental Model in a Sample of Community Adults. Collabra Psychology, 10(1). https://doi.org/10.1525/collabra.121392
Demartini, B., Wiedemann, F., Faggioli, R., & Nisticò, V. (2025). Prevalence and Characteristics of Attention Deficit Hyperactivity Disorder in Adults With Autism Spectrum Disorders Without Intellectual Disabilities. European Psychiatry, 68(S1), S355-S356. https://doi.org/10.1192/j.eurpsy.2025.750
Guo, C. (2024). Specific Impairments and Challenges in Women With ADHD. Journal of Education Humanities and Social Sciences, 29, 34-39. https://doi.org/10.54097/vrh8jk90
Halbe, E., Heger, A. S., Kolf, F., Hüpen, P., Bergmann, M., Harrison, B. J., Davey, C. G., Philipsen, A., & Lux, S. (2024). Sex Differences in Physiological Correlates of Affectively Driven Decision-Making Behavior in Adult ADHD. BMC psychiatry, 24(1). https://doi.org/10.1186/s12888-024-06040-3
Hanan, M., & Kelbrick, M. (2024). Improving Quality of Care for Patients With Attention-Deficit/Hyperactivity Disorder in an Early Intervention for Psychosis Service. BJPsych Open, 10(S1), S142-S143. https://doi.org/10.1192/bjo.2024.377
Javid, A., Ahmed, M., & Sikandar, E. (2024). Breaking Ground on ADHD Diagnosis in Pakistan. Journal of the Pakistan Medical Association, 74(4), 613-613. https://doi.org/10.47391/jpma.10119
Jong, M. d., Wynchank, D. S. M. R., Andel, E. v., Beekman, A. T., & Kooij, J. J. S. (2023). Female-Specific Pharmacotherapy in ADHD: Premenstrual Adjustment of Psychostimulant Dosage. Frontiers in Psychiatry, 14. https://doi.org/10.3389/fpsyt.2023.1306194
Maciver, D. (2025). Are We Getting Better at Identifying and Diagnosing Neurodivergent Girls and Women? Insights Into Sex Ratios and Age of Diagnosis From Clinical Population Data in Scotland. Autism. https://doi.org/10.1177/13623613251383343
Maulida, A. R., Setiawati, Y., Avidar, Y. P., Amanda, B., & Ashari, F. Y. (2025). Exploration of ADHD in Females: Review on Symptomatic Presentation and Effect of Late Diagnosis or Misdiagnosis on Women’s Quality of Life. International Journal of Scientific Advances, 6(3). https://doi.org/10.51542/ijscia.v6i3.35
Murniati, R., Sholihatin, I., Khalda, Y. I., & Sulistiawangi. (2024). Diagnose and Treatment of ADHD in Adult Woman: A Literature Review. Jurnal Biologi Tropis, 24(1b), 335-341. https://doi.org/10.29303/jbt.v24i1b.7954
oban, D., Tan, Ö., & mu, b. (2024). Clinical and Sociodemographic Differences in Adult Women and Men With Obsessive-Compulsive Disorder. Psychiatry and Behavioral Sciences, 14(3), 167. https://doi.org/10.5455/pbs.20240618101957
Oroian, B. A., Costandache, G., Popescu, E.-C., Nechita, P., & Szalontay, A. S. (2024). The Uncharted Territory of Female Adult ADHD: A Comprehensive Review. European Psychiatry, 67(S1), S299-S300. https://doi.org/10.1192/j.eurpsy.2024.624
Ramalheira, F., Gonçalves, F. R., Vieira, S. C. M., Cohen, R., Cameira, M., & Robalo, P. (2025). Mind the Gap: Gender Differences in Attention Deficit and Hyperactivity Disorder. European Psychiatry, 68(S1), S260-S260. https://doi.org/10.1192/j.eurpsy.2025.576
Smith, S., & McVeigh, J. (2025). Perceptions of Stigma and Social Inclusion Amongst a Sample of University Students With ADHD in Ireland. Disabilities, 5(1), 24. https://doi.org/10.3390/disabilities5010024
Song, S. (2024). The Role of Cultural Factors in Attention Deficit Hyperactivity Disorder (ADHD) Diagnosis in Children in Nigeria. Studies in Psychological Science, 2(1), 40-47. https://doi.org/10.56397/sps.2024.03.05
Visser, M. J., Peters, R. M., & Luman, M. (2024). Understanding ADHD-related Stigma: A Gender Analysis of Young Adult and Key Stakeholder Perspectives. Neurodiversity, 2. https://doi.org/10.1177/27546330241274664
Williams, T., Barclay, I., Jones, R. B., Livingston, L. A., Agha, S. S., Ford, T., John, A., Sayal, K., Thapar, A., & Martin, J. (2025). Reflections on the Manifestation of Attention-Deficit Hyperactivity Disorder in Girls From Young Adults With Lived Experiences: A Qualitative Study. The British Journal of Psychiatry, 227(5), 775-782. https://doi.org/10.1192/bjp.2025.10376
Younes, S., Hajj, A., Sacre, H., Mourad, N., Akel, M., Haddad, C., Sakr, F., Zeenny, R. M., & Salameh, P. (2024). Exploring ADHD Understanding and Stigma: Insights From an Online Survey in Lebanon. PLoS One, 19(11), e0310755. https://doi.org/10.1371/journal.pone.0310755
Young, S., Uysal, Ö., Kahle, J., Gudjónsson, G. H., Hollingdale, J., Cortese, S., Sakalli-Kani, A., Greer, B., Cocallis, K., Sylver, N., Yılmaz, U., Semerci, B., & Kılıç, Ö. (2024). A Systematic Review and Meta-Analysis Comparing the Severity of Core Symptoms of Attention-Deficit Hyperactivity Disorder in Females and Males. Psychological medicine, 54(14), 3763-3784. https://doi.org/10.1017/s0033291724001600