The Effectiveness of Spiritual Self-Care on Death Anxiety and Hope for Life in Cardiac Patients
Keywords:
Spiritual self-care, Death Anxiety, hope for lifeAbstract
Objective: This study aimed to investigate the effectiveness of a structured spiritual self-care program in reducing death anxiety and enhancing hope for life among female patients with cardiovascular disease.
Methods and Materials: The research employed a quasi-experimental pretest–posttest design with a control group and a three-month follow-up. The statistical population consisted of female patients referred to the cardiology ward of Sina Hospital in Semnan in 2024. A total of 45 participants were recruited through convenience sampling and randomly assigned to three groups (two intervention groups and one control group). Inclusion and exclusion criteria were strictly applied, and participants provided written informed consent. Data were collected using the Templer Death Anxiety Scale and the Miller Hope Scale. The intervention included structured sessions of spiritual self-care practices such as prayer, gratitude, patience, and reflection. Data analysis was conducted using repeated-measures analysis of variance (ANOVA) with Greenhouse–Geisser corrections through SPSS version 26.
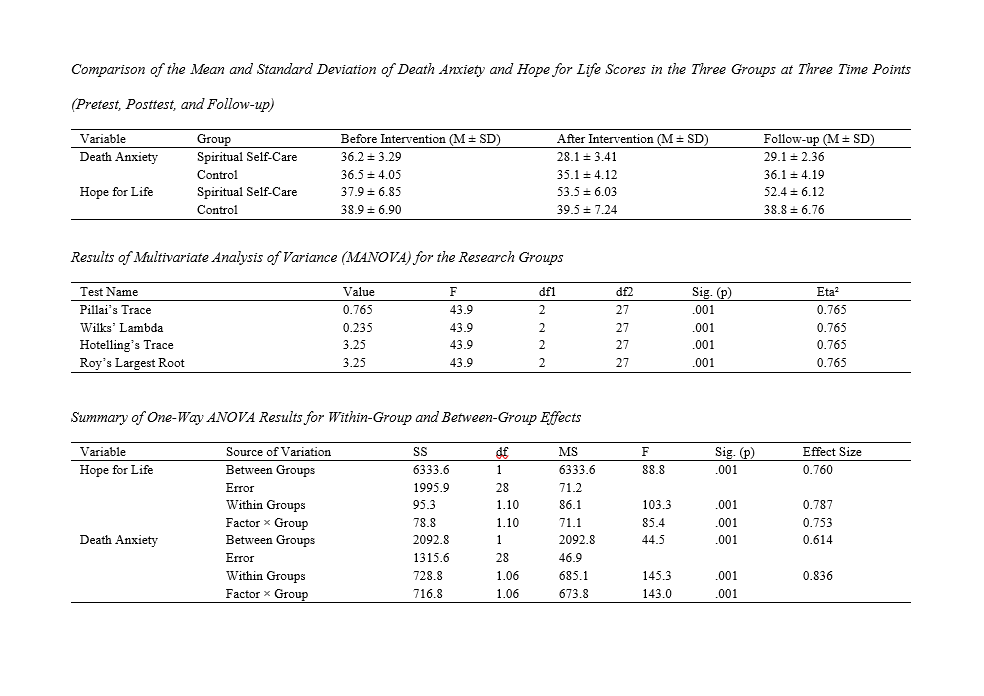
Findings: The results revealed significant between-group differences for both dependent variables. Results showed that spiritual self-care significantly reduced death anxiety (Wilks’ Lambda = 0.235, F(2,27) = 43.9, p < .001, η² = 0.765) and significantly increased hope for life (F(1,28) = 88.8, p < .001, η² = 0.760) in the intervention groups compared to the control group. Pairwise comparisons confirmed that these improvements were sustained at the three-month follow-up, indicating the stability of intervention effects.
Conclusion: The findings suggest that spiritual self-care interventions are effective in reducing existential distress and fostering hope among cardiac patients. Incorporating spiritual self-care into cardiac rehabilitation and psychological support programs may enhance holistic patient care and improve long-term psychological resilience.
Downloads
References
Basu, S., & Sharma, N. (2021). Diabetes self-care in primary health facilities in India-challenges and the way forward. World Journal of Diabetes, 10(6), 341. https://doi.org/10.4239/wjd.v10.i6.341
Batı, S., Polat, H. T., & Akkuş, H. (2024). Determination of the relationship between self-care agency and death anxiety among elderly individuals. OMEGA-Journal of Death and Dying, 89(4), 1535-1550. https://doi.org/10.1177/00302228221095907
Borba, A. K. D. O. T., Arruda, I. K. G., Marques, A. P. D. O., Leal, M. C. C., & Diniz, A. D. S. (2022). Knowledge and attitude about diabetes self-care of older adults in primary health care. Ciência & Saúde Coletiva, 24, 125-136. https://doi.org/10.1590/1413-81232018241.35052016
Chen, T. Y., Kao, C. W., Cheng, S. M., & Liu, C. Y. (2023). Factors influencing self-care among patients with primary hypertension: Path analysis of mediating roles of self-efficacy and depressive symptoms. European Journal of Cardiovascular Nursing. https://doi.org/10.1093/eurjcn/zvad011
Evans, K. (2025). Trauma-informed self-care practices in speech-language pathology and related professions: A scoping review. Topics in Language Disorders, 45(1), 41-59. https://doi.org/10.1097/TLD.0000000000000360
Harris, M., & Brackett, A. (2023). Self-Care: When and How. In General Surgery Residency Survival Guide (pp. 175-177). Springer International Publishing. https://doi.org/10.1097/MLR.0000000000001814
Hermanns, N., Ehrmann, D., Shapira, A., Kulzer, B., Schmitt, A., & Laffel, L. (2022a). Coordination of glucose monitoring, self-care nalyzin and mental health: achieving precision monitoring in diabetes. Diabetologia, 1-12. https://doi.org/10.1007/s00125-022-05685-7
Hermanns, N., Ehrmann, D., Shapira, A., Kulzer, B., Schmitt, A., & Laffel, L. (2022b). Coordination of glucose monitoring, self-care nalyzin and mental health: achieving precision monitoring in diabetes. Diabetologia, 65(11), 1883-1894. https://doi.org/10.1007/s00125-022-05685-7
Jordan, M. (2023). The power of connection: Self-care strategies of social wellbeing. Journal of Interprofessional Education & Practice, 100586. https://doi.org/10.1016/j.xjep.2022.100586
Kolasa, J., Frączek-Jucha, M., Grabowski, M., Jankowska, E. A., Lelonek, M., Pawlak, A., & Nessler, J. (2022). A quasi-experimental study examining a nurse-led educational program to improve disease knowledge and self-care for patients with acute decompensated heart failure with reduced ejection fraction. Advances in Clinical and Experimental Medicine, 31(3), 267-275. https://doi.org/10.17219/acem/143989
Lee, H., & Cho, M. K. (2025). Effects of Shared Decision-Making, Health Literacy, and Self-Care Knowledge on Self-Care Behavior Among Hemodialysis Patients in Korea: A Cross-Sectional Survey. Healthcare,
Lewis, S., Willis, K., Bismark, M., & Smallwood, N. (2022). A time for self-care? Frontline health workers' strategies for managing mental health during the COVID-19 pandemic. SSM-Mental Health, 2, 100053. https://doi.org/10.1016/j.ssmmh.2021.100053
Liou, H. L., Chen, H. I., Hsu, S. C., Lee, S. C., Chang, C. J., & Wu, M. J. (2015). The effects of a self-care program on patients with heart failure. Journal of the Chinese Medical Association, 78(11), 648-656. https://doi.org/10.1016/j.jcma.2015.06.004
Lu, F., Wong, C. K. H., Tse, E. T. Y., Ng, A. P. P., Li, L., Lam, J. S. M., & Lam, C. L. K. (2023). The Impact of a Health Empowerment Program on Self-Care Enablement and Mental Health among Low-Income Families: Evidence from a 5 Year Cohort Study in Hong Kong. International journal of environmental research and public health, 20(6), 5168. https://doi.org/10.3390/ijerph20065168
Martens, T. W., Willis, H. J., Bergenstal, R. M., Kruger, D. F., Karslioglu-French, E., & Steenkamp, D. W. (2025). A Randomized Controlled Trial Using Continuous Glucose Monitoring to Guide Food Choices and Diabetes Self-Care in People with Type 2 Diabetes not Taking Insulin. Diabetes Technology & Therapeutics. https://doi.org/10.1089/dia.2024.0579
Miller, S. T., Akohoue, S. A., Murry, V. M., Tabatabai, M., Wilus, D., & Foxx, A. (2023). SISTER (Sisters inspiring sisters to engage in relevant diabetes self-care) diabetes study: Protocol for diabetes medical nutrition therapy randomized clinical trial among African American women. Contemporary Clinical Trials, 125, 107052. https://doi.org/10.1016/j.cct.2022.107052
Oliveira, D., Zarit, S. H., & Orrell, M. (2023). Health-promoting self-care in family caregivers of people with dementia: the views of multiple stakeholders. The Gerontologist, 59(5), e501-e511. https://academic.oup.com/gerontologist/article-abstract/59/5/e501/5430246
Öztürk, Z., Turan, G. B., & Aksoy, M. (2023). The Effect of Spiritual Well-Being on Self-care Agency in Chronic Obstructive Pulmonary Patients in Turkey: The Mediating Role of Psychological Resilience. Journal of religion and health. https://doi.org/10.1007/s10943-023-01961-x
Park, J., & McElveen, K. (2025). Optimal Self-Care for Surgeons: Sleep, Diet, and Exercise. The American Surgeon™, 91(1), 161-164. https://doi.org/10.1177/00031348241269422
Popoviciu, M. S., Marin, V. N., Vesa, C. M., Stefan, S. D., Stoica, R. A., Serafinceanu, C., & Stoian, A. P. (2022). Correlations between diabetes mellitus self-care activities and glycaemic control in the adult population: a cross-sectional study. Healthcare, 10(1), 174. https://doi.org/10.3390/healthcare10010174
Riegel, B., Barbaranelli, C., Quinn, R., Matus, A., Stawnychy, M. A., & Hirschman, K. B. (2024). Psychometric analysis of the health self-care neglect scale. Journal of Cardiovascular Nursing, 39(3), 288-295. https://doi.org/10.1097/JCN.0000000000001047
Rodríguez-Ramos, P. A., Aguilera-Ávila, L., & Gonzalez-Mendez, R. (2025). Development and Validation of the Barriers to Professional Self-Care Scale (BPS-CS). Social Work, 70(1), 69-79. https://doi.org/10.1093/sw/swae052
Sands, L. P., Lee, L., Zhu, X., Khan, M., & Du, P. (2025). Risks and Outcomes of New Onset of Unmet Need for Mobility and Self-care Daily Activities. The Gerontologist, 65(2), gnae154. https://doi.org/10.1093/geront/gnae154
Sari, E. A., Mirwanti, R., Herliani, Y. K., & Pratiwi, S. H. (2025). Self-Care Behavior Based on Knowledge of Patients with Hypertension: A Cross-Sectional Study. Vascular Health and Risk Management, 17-24. https://doi.org/10.2147/VHRM.S489688
Situmorang, D. D. B., & Situmorang, D. D. B. (2022). 'Rapid Counseling' with single-session therapy for patients with COVID-19: An alternative treatment before doing mental health self-care strategy with meditation. Journal of Public Health, 44(4), e640-e641. https://doi.org/10.1093/pubmed/fdab345
Spors, V., & Kaufman, I. (2021). Respawn, Reload, Relate: Exploring the Self-Care Possibilities for Mental Health in Games through a Humanistic Lens. Proceedings of the Acm on Human-Computer Interaction, 5(CHI PLAY), 1-31. https://doi.org/10.1145/3474690
Steele, V., & Grajo, L. (2023). A Preliminary Study on the Content Validity of the Family Assessment of Quality in Self-Care Engagement. The American journal of occupational therapy, 77(2), 7702185030. https://doi.org/10.5014/ajot.2023.050112
Town, R., Hayes, D., Moore, A., Fonagy, P., & Stapley, E. (2023). Self-management, self-care, and self-help in young people with emotional problems: a scoping review. European Child and Adolescent Psychiatry. https://doi.org/10.1007/s00787-022-02134-z
Ucciero, S., Lacarbonara, F., Durante, A., Torino, F., Uchmanowicz, I., Vellone, E., & Di Nitto, M. (2024). Predictors of self-care in patients with cancer treated with oral anticancer agents: A systematic review. PLoS One, 19(9), e0307838. https://doi.org/10.1371/journal.pone.0307838
Van Rijn, M. M., Jaarsma, T., de Man-van Ginkel, J. M., & Weldam, S. W. (2023). Association between self-care and resilience: A cross-sectional study in heart failure patients. Journal of Cardiovascular Nursing, 38(2), E70-E77. https://doi.org/10.1097/JCN.0000000000000908
Vega-Martínez, M. D. C., López-Martínez, C., & Del-Pino-Casado, R. (2025). Sense of coherence and self-care in people with diabetes: systematic review. medRxiv. https://doi.org/10.1101/2025.01.16.25320434
Wan, D. W. J., Goh, L. S. H., Teo, M. Y. K., Loh, C. J. L., Yak, G. H. K., Lee, J. J. H., & Krishna, L. K. R. (2024). Enhancing self-care education amongst medical students: a systematic scoping review. BMC Medical Education, 24(1), 37. https://doi.org/10.1186/s12909-023-04965-z
White, M. L. (2016). Spirituality Self-Care Practices as a Mediator between Quality of Life and Depression. Religions, 7(5), 54. https://doi.org/10.3390/rel7050054
Woda, A., Belknap, R. A., Haglund, K., Sebern, M., & Lawrence, A. (2015). Factors influencing self-care behaviors of African Americans with heart failure: A photovoice project. Heart & Lung, 44(1), 33-38. https://doi.org/10.1016/j.hrtlng.2014.09.001
Zhong, B., & Xie, L. (2023). Making “Joy Pie” to stay joyful: self-care interventions alleviate college students’ mental health challenges. International journal of environmental research and public health, 20(5), 3823. https://www.mdpi.com/1660-4601/20/5/3823