Exploring the Dimensions of Motivation in Stroke Survivors During Physical Rehabilitation: A Qualitative Inquiry
Keywords:
Stroke rehabilitation, Motivation, Qualitative research, Patient engagement, Social support, Thematic analysisAbstract
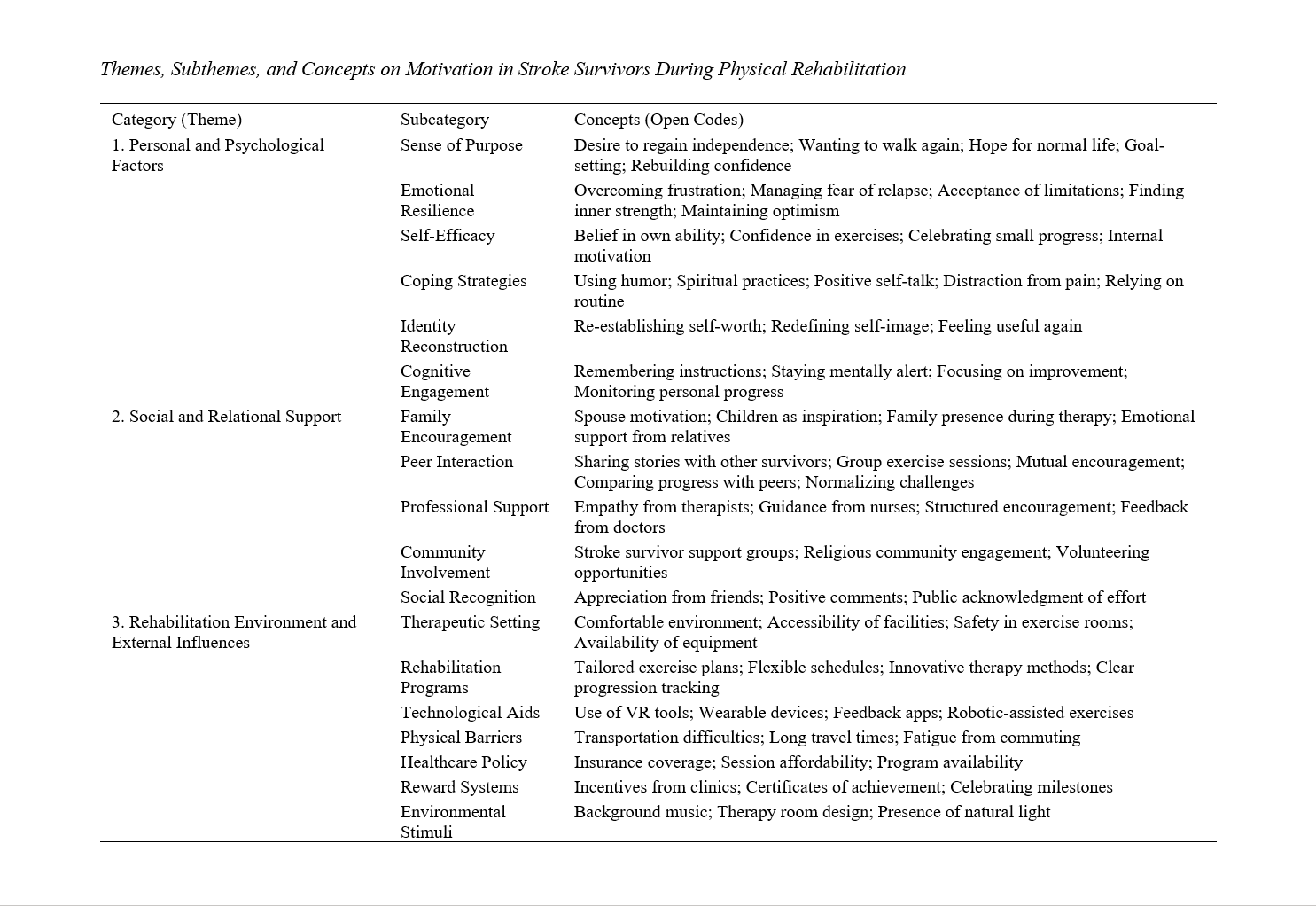
The objective of this study was to explore the dimensions of motivation in stroke survivors during physical rehabilitation, focusing on the personal, social, and environmental factors that shape engagement and recovery. This qualitative study employed an exploratory design to investigate motivational experiences of stroke survivors. Twenty participants (11 men and 9 women, aged 38–72) were recruited purposively from rehabilitation centers across the United States. Semi-structured interviews were conducted, each lasting 45–75 minutes, and data collection continued until theoretical saturation was reached. Interviews were audio-recorded, transcribed verbatim, and analyzed using thematic analysis with NVivo 14 software. Coding was carried out iteratively, with two researchers independently coding transcripts to ensure reliability, followed by consensus meetings to finalize themes. Three overarching themes emerged from the data. The first, personal and psychological factors, encompassed subthemes such as sense of purpose, emotional resilience, self-efficacy, coping strategies, identity reconstruction, and cognitive engagement. The second, social and relational support, included family encouragement, peer interaction, professional support, community involvement, and social recognition. The third, rehabilitation environment and external influences, comprised therapeutic setting, individualized programs, technological aids, physical and financial barriers, healthcare policies, reward systems, and environmental stimuli. Participants described motivation as a dynamic construct shaped by internal beliefs, relational networks, and systemic conditions, with direct quotations illustrating these lived experiences. The findings demonstrate that motivation in stroke rehabilitation is multidimensional, integrating psychological, social, and environmental domains. Recognizing and addressing these interconnected factors can enhance rehabilitation engagement, optimize functional outcomes, and promote holistic recovery. The study underscores the need for patient-centered, socially embedded, and technologically supported rehabilitation strategies.
Downloads
References
Andriani, M., & Agustriyani, F. (2021). Hubungan Dukungan Keluarga Dengan Motivasi Pasien Pasca Stroke Melakukan ROM Aktif Di RSUD DR. A Dadi Tjokrodipo. Journal of Current Health Sciences, 1(1), 7-12. https://doi.org/10.47679/jchs.v1i1.2
Baihaqi, M. N., Suminar, J. R., & Prasanti, D. (2024). Pola Komunikasi Anggota Keluarga Dengan Penyandang Stroke Iskemik Sebagai Upaya Pemulihan. Humanus, 1(3), 444-458. https://doi.org/10.62180/185q3872
Caine, S., Alaverdashvili, M., Colbourne, F., Muir, G. D., & Paterson, P. G. (2024). A Modified Rehabilitation Paradigm Bilaterally Increased Rat Extensor Digitorum Communis Muscle Size but Did Not Improve Forelimb Function After Stroke. PLoS One, 19(4), e0302008. https://doi.org/10.1371/journal.pone.0302008
Cern, Y. S., & Ze, Y. S. (2023). The Design of Stroke Rehabilitation Using Artificial Intelligence K.A.K.I (Kinesthetic Augmented Kinematic Inference). Jurnal Kejuruteraan, 35(6), 1383-1391. https://doi.org/10.17576/jkukm-2023-35(6)-11
Conforto, A. B., Liew, S. L., Luft, A. R., Kitago, T., Bernhardt, J., & Arenillas, J. F. (2022). Editorial: Understanding Stroke Recovery to Improve Outcomes: From Acute Care to Chronic Rehabilitation. Frontiers in Neurology, 13. https://doi.org/10.3389/fneur.2022.1021033
Elmanowski, J., Kleynen, M., Geers, R., Rovelo-Ruiz, G., Geurts, E., Coninx, K., Verbunt, J., & Seelen, H. A. (2023). Task-Oriented Arm Training for Stroke Patients Based on Remote Handling Technology Concepts: A Feasibility Study. Technology and Health Care, 31(5), 1593-1605. https://doi.org/10.3233/thc-220465
Kawano, M., Takamura, Y., Tachihara, M., Yokota, K., & Yozu, A. (2021). The Relationship Between Motivation for Rehabilitation and Sense of Agency in Patients With Cerebrovascular Disease, and Nurse Support for Patient Agency. International Journal of Affective Engineering, 20(3), 143-151. https://doi.org/10.5057/ijae.ijae-d-20-00029
Kumar, A., Fang, Q., & Pirogova, E. (2021). The Influence of Psychological and Cognitive States on Error-Related Negativity Evoked During Post-Stroke Rehabilitation Movements. Biomedical Engineering Online, 20(1). https://doi.org/10.1186/s12938-021-00850-2
Li, W., Zhu, G., Lu, Y., Wu, J., Fu, Z., Tang, J., Zhang, G., & Xu, D. (2024). The Relationship Between Rehabilitation Motivation and Upper Limb Motor Function in Stroke Patients. Frontiers in Neurology, 15. https://doi.org/10.3389/fneur.2024.1390811
Melnikova, E. A., Ткаченко, Г. А., Tsvetkova, E. M., Starkova, E. Y., Vladimirova, N. N., & Litau, V. Y. (2024). The Influence of Patient Motivation on the Motor Function Restoration During Stroke Recovery. Preliminary Results of a Clinical Study. Physical and Rehabilitation Medicine Medical Rehabilitation, 6(2), 122-130. https://doi.org/10.36425/rehab629104
Mercer, E., Sherfey, E., Ogbu, C., & Riley, E. A. (2022). Effects of CPAP on Language Recovery in Post-Stroke Aphasia: A Review of Recent Literature. Brain Sciences, 12(3), 379. https://doi.org/10.3390/brainsci12030379
Mersha, M. D., Hubbard, R., & Zeiler, S. R. (2024). Alternate Day Fasting Leads to Improved Post-Stroke Motor Recovery in Mice. Neurorehabilitation and Neural Repair, 38(3), 187-196. https://doi.org/10.1177/15459683241232680
Moon, K. J. (2022). A Qualitative Study on the Rehabilitation Recovery Experience of Stroke Patients and Spouses. Korean Society for Rehabilitation of Persons With Disabilities, 26(3), 51-72. https://doi.org/10.16884/jrr.2022.26.3.51
Pallesen, H., Aadal, L., Moe, S., & Arntzen, C. (2019). Gateway to Recovery: A Comparative Analysis of Stroke Patients’ Experiences of Change and Learning in Norway and Denmark. Rehabilitation Research and Practice, 2019, 1-14. https://doi.org/10.1155/2019/1726964
Rabadi, M. H., & Xu, C. (2025). Motivation in Veterans With an Acute/Subacute Ischemic Stroke Did Not Improve Cognition and Functional Motor Recovery but Reduced Deaths. European Journal of Physical and Rehabilitation Medicine, 61(1). https://doi.org/10.23736/s1973-9087.24.08563-0
Sato, C., Tanji, K., Shimoyama, S., Chiba, M., Misaki, M., Koeda, S., Koshi, S., Akahira, K., & Yamada, J. (2020). Effects of Voluntary and Forced Exercises on Motor Function Recovery in Intracerebral Hemorrhage Rats. NeuroReport, 31(2), 189-196. https://doi.org/10.1097/wnr.0000000000001396
Tan, M., Li, H., & Wang, X. (2023). Analysis of the Current Status of Rehabilitation Motivation and Its Influencing Factors in Older Adults With Stroke: A Cross-Sectional Study. Frontiers in Aging Neuroscience, 15. https://doi.org/10.3389/fnagi.2023.1186681
Tun, S. S. H., Wanpen, S., & Nualnetr, N. (2024). Influential Factors Contributing to Stroke Recovery: A Review. Iseth, 1282-1287. https://doi.org/10.23917/iseth.4222
Vasu, D. T., & Pang, Y. G. (2024). Relationship Between Locus of Control and Health-Related Quality of Life in Chronic Stroke Patients: A Cross-Sectional Study. Bulletin of Faculty of Physical Therapy, 29(1). https://doi.org/10.1186/s43161-024-00241-3
Waddell, K. J., Strube, M., Tabak, R. G., Haire‐Joshu, D., & Lang, C. E. (2019). Upper Limb Performance in Daily Life Improves Over the First 12 Weeks Poststroke. Neurorehabilitation and Neural Repair, 33(10), 836-847. https://doi.org/10.1177/1545968319868716
Waddell, K. J., Tabak, R. G., Strube, M., Haire‐Joshu, D., & Lang, C. E. (2019). Belief, Confidence, and Motivation to Use the Paretic Upper Limb in Daily Life Over the First 24 Weeks After Stroke. Journal of Neurologic Physical Therapy, 43(4), 197-203. https://doi.org/10.1097/npt.0000000000000287