Exploring Dimensions of Trauma-Linked Somatic Complaints in Refugees: A Qualitative Study in Canada
Keywords:
Refugees, Trauma, Somatic complaints, Qualitative research, Canada, Mental health, Coping strategies, Post-migration stressorsAbstract
Objective: This study aimed to explore the dimensions of trauma-linked somatic complaints among refugees, focusing on how trauma is embodied, expressed, and managed in the context of displacement.
Methods and Materials: A qualitative research design was employed, using semi-structured in-depth interviews with 17 refugees residing in Canada. Participants were recruited through community networks and refugee support organizations. Interviews, lasting 60–90 minutes, were conducted with the aid of professional interpreters where necessary and continued until theoretical saturation was reached. All interviews were audio-recorded, transcribed verbatim, and analyzed using NVivo 14 software. A thematic analysis approach was applied, involving iterative coding, categorization, and theme development to capture the range of trauma-linked somatic experiences.
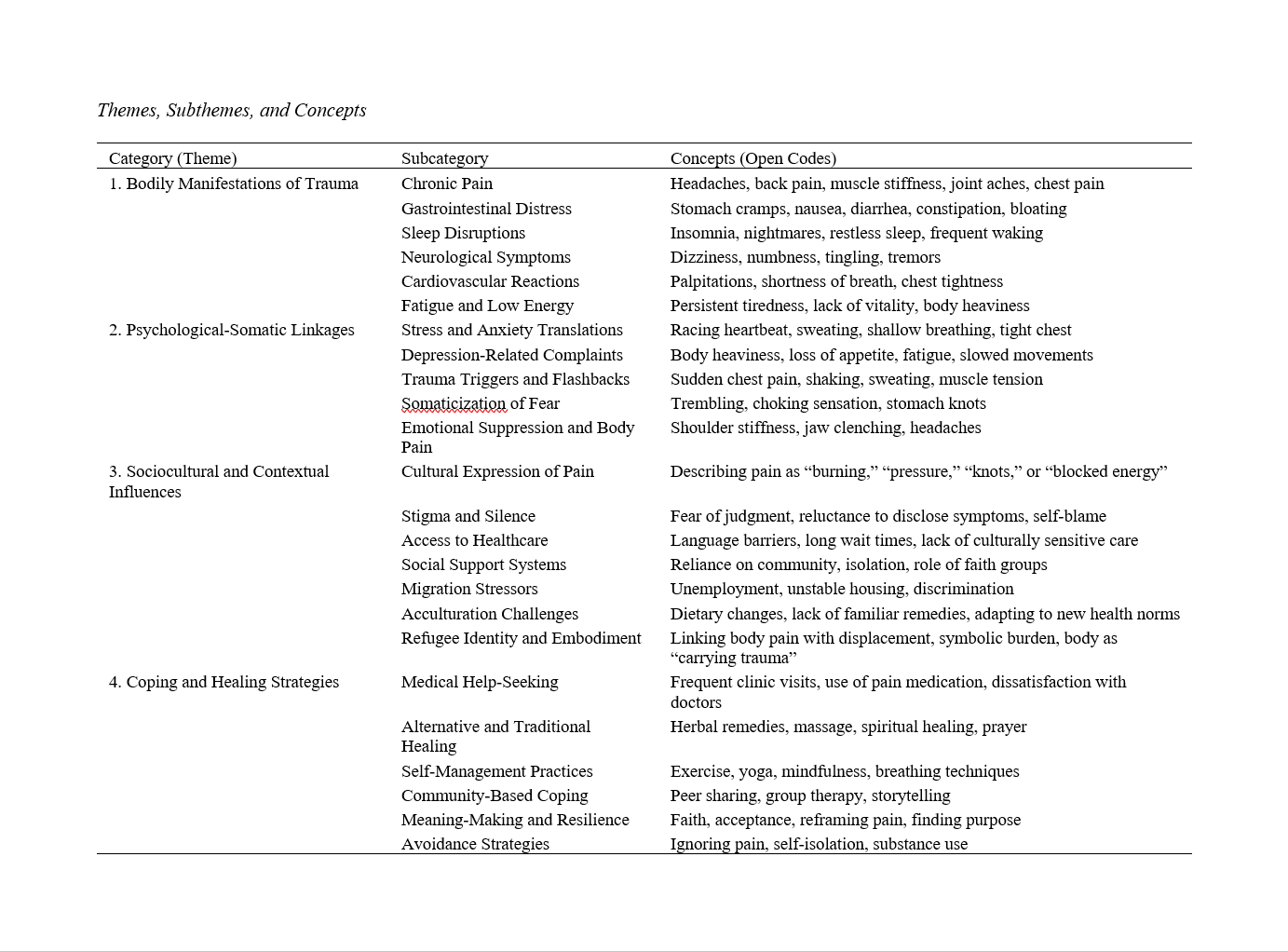
Findings: Four overarching themes emerged from the analysis: (1) Bodily manifestations of trauma, including chronic pain, gastrointestinal distress, sleep disturbances, neurological symptoms, cardiovascular complaints, and persistent fatigue; (2) Psychological-somatic linkages, where anxiety, depression, flashbacks, and emotional suppression were embodied through physical discomforts; (3) Sociocultural and contextual influences, including cultural idioms of distress, stigma, access barriers to healthcare, post-migration stressors, and the role of community and faith; and (4) Coping and healing strategies, ranging from medical help-seeking and alternative remedies to mindfulness, community-based support, resilience-building, and avoidance. Participants’ narratives highlighted the embodied nature of trauma and the interplay between pre-migration trauma and post-migration challenges in shaping somatic complaints.
Conclusion: The study underscores that trauma-linked somatic complaints among refugees are complex, multifaceted, and shaped by cultural and contextual factors. Recognizing these complaints as legitimate trauma expressions is crucial for trauma-informed healthcare and fair asylum adjudication. Integrating medical, psychological, and social approaches, alongside culturally sensitive and community-based interventions, is essential to address the embodied dimensions of refugee trauma.
Downloads
References
Aarts, R., Wanrooij, L. L. v., Bloemen, E., & Smid, G. E. (2019). Expert Medico-Legal Reports: The Relationship Between Levels of Consistency and Judicial Outcomes in Asylum Seekers in the Netherlands. Torture Journal, 29(1), 36-46. https://doi.org/10.7146/torture.v29i1.111205
Bishop, S. (2021). Intercultural Communication, the Influence of Trauma, and the Pursuit of Asylum in the United States. Journal of Ethnic and Cultural Studies, 8(2), 187-208. https://doi.org/10.29333/ejecs/667
Cannon, B., & Murphy, S. (2024). ‘We’re Not Right-Wing or Racist But…’: Far-Right Myth and Distributive Conflict in Asylum Seeker Related Protest in the Republic of Ireland, November 2022–July 2023. Irish Journal of Sociology, 32(1-2), 225-234. https://doi.org/10.1177/07916035241259252
Cossu, G., Preti, A., & Carta, M. G. (2018). Treatment of Mental Health Problems in Refugees and Asylum Seekers. 289-304. https://doi.org/10.1093/med/9780198792994.003.0033
Cranwell, G. (2024). A Primer on Trauma-Informed Practice in Refugee Law. Bond Law Review, 36(1). https://doi.org/10.53300/001c.123295
Cvikl, L., & Flander, B. (2023). Asylum and Refugee Issues in the Case Law of the Constitutional Court of the Republic of Slovenia. Law Identity and Values, 3(2), 51-87. https://doi.org/10.55073/2023.2.51-87
Führer, A., Eichner, F., & Stang, A. (2016). Morbidity of Asylum Seekers in a Medium-Sized German City. European Journal of Epidemiology, 31(7), 703-706. https://doi.org/10.1007/s10654-016-0148-4
Garoff, F., Skogberg, N., Klemettilä, A., Lilja, E., Omar, A. A. H., Snellman, O., & Castañeda, A. E. (2021). Mental Health and Traumatization of Newly Arrived Asylum Seeker Adults in Finland: A Population-Based Study. International journal of environmental research and public health, 18(13), 7160. https://doi.org/10.3390/ijerph18137160
Grupp, F., Moro, M. R., Skandrani, S., & Mewes, R. (2022). Coping With Trauma and Symptoms of Post-Traumatic Stress Disorder: Exploring Intentions and Lay Beliefs About Appropriate Strategies Among Asylum-Seeking Migrants From Sub-Saharan Africa in Germany. International journal of environmental research and public health, 19(3), 1783. https://doi.org/10.3390/ijerph19031783
Ingram, J., Lyford, B., McAtamney, A., & Fitzpatrick, S. (2022). Preventing Suicide in Refugees and Asylum Seekers: A Rapid Literature Review Examining the Role of Suicide Prevention Training for Health and Support Staff. International Journal of Mental Health Systems, 16(1). https://doi.org/10.1186/s13033-022-00534-x
Khouani, J., Blatrix, L., Tinland, A., Jego, M., Gentile, G., Fond, G., Loundou, A., Fromentin, M., & Auquier, P. (2022). Health Status of Recently Arrived Asylum Seekers in Their Host Country: Results of a Cross-Sectional Observational Study. BMC public health, 22(1). https://doi.org/10.1186/s12889-022-14095-8
Kissane, M., Szymanski, L., Upthegrove, R., & Katona, C. (2014). Complex Posttraumatic Stress Disorder in Traumatised Asylum Seekers: A Pilot Study. The European Journal of Psychiatry, 28(3), 137-144. https://doi.org/10.4321/s0213-61632014000300001
Lashwood, H., Toynbee, M., Hillier, B., & Tracy, D. K. (2025). Impact of the Increased Asylum Seeker Population on a UK Mental Health Crisis Service. BJPsych International, 1-8. https://doi.org/10.1192/bji.2025.6
Li, S. S. Y., Liddell, B. J., & Nickerson, A. (2016). The Relationship Between Post-Migration Stress and Psychological Disorders in Refugees and Asylum Seekers. Current psychiatry reports, 18(9). https://doi.org/10.1007/s11920-016-0723-0
Misra, S. (2020). A Critical Reflexive Account From Participatory Theater With Asylum Seekers: Lessons for Framing Trauma and Resilience in Refugee Status Determination. Frontiers in Communication, 5. https://doi.org/10.3389/fcomm.2020.00040
Molyneux, K., & Singer, E. (2024). Asylum Seekers and the Role of the Acute Care Physician. Journal of the American College of Emergency Physicians Open, 5(3), e13196. https://doi.org/10.1002/emp2.13196
Morgan, G., Melluish, S., & Welham, A. (2017). Exploring the Relationship Between Postmigratory Stressors and Mental Health for Asylum Seekers and Refused Asylum Seekers in the UK. Transcultural Psychiatry, 54(5-6), 653-674. https://doi.org/10.1177/1363461517737188
Newman, L. (2013). Seeking Asylum—Trauma, Mental Health, and Human Rights: An Australian Perspective. Journal of Trauma & Dissociation, 14(2), 213-223. https://doi.org/10.1080/15299732.2013.724342
Ngo, T., & Hodes, M. (2019). Pervasive Refusal Syndrome in Asylum-Seeking Children: Review of the Current Evidence. Clinical Child Psychology and Psychiatry, 25(1), 227-241. https://doi.org/10.1177/1359104519846580
Nissen, R. P., Frederiksen, H. W., Brande, S. E., & Nørredam, M. (2022). The General Health Status of Newly Arrived Asylum Seekers in Denmark. Scandinavian Journal of Public Health, 51(3), 463-471. https://doi.org/10.1177/14034948221136366
Oehri, J., Chernet, A., Merten, S., Sydow, V., & Paris, D. H. (2023). Improving Primary Healthcare Access for Asylum Seekers and Refugees: A Qualitative Study From a Swiss Family Physician Perspective. Journal of Primary Care & Community Health, 14. https://doi.org/10.1177/21501319231181878
Oxford, C. (2023). The Gory Details: Asylum, Sexual Assault, and Traumatic Memory. Sexes, 4(2), 188-221. https://doi.org/10.3390/sexes4020015
Pfortmueller, C. A., Schwetlick, M., Mueller, T., Lehmann, B., & Exadaktylos, A. K. (2016). Adult Asylum Seekers From the Middle East Including Syria in Central Europe: What Are Their Health Care Problems? PLoS One, 11(2), e0148196. https://doi.org/10.1371/journal.pone.0148196
Pineda, L., & Punsky, B. (2024). Mental Health as the Cornerstone of Effective Medical-Legal Partnerships for Asylum-Seekers: The Terra Firma Model. Psychological Trauma Theory Research Practice and Policy, 16(Suppl 2), S417-S425. https://doi.org/10.1037/tra0001343
Reebs, A., Yuval, K., Hadash, Y., Gebremariam, S., & Bernstein, A. (2020). Mindfulness-Based Trauma Recovery for Refugees (MBTR-R): Randomized Waitlist-Control Evidence of Efficacy and Safety. https://doi.org/10.31231/osf.io/jyhwa
Saadi, A., Hampton, K., Assis, M. V. d., Mishori, R., Habbach, H., & Haar, R. J. (2021). Associations Between Memory Loss and Trauma in US Asylum Seekers: A Retrospective Review of Medico-Legal Affidavits. PLoS One, 16(3), e0247033. https://doi.org/10.1371/journal.pone.0247033
Saadi, A., Williams, J., Parvez, A., Alegrı́a, M., & Vranceanu, A. M. (2023). Head Trauma in Refugees and Asylum Seekers. Neurology, 100(21). https://doi.org/10.1212/wnl.0000000000207261
Tessitore, F. (2022). The Asylum Seekers Photographic Interview (ASPI): Evaluation of a New Method to Increase Nigerian Asylum Seekers’ Narrative Meaning-Making After Trauma. Psychological Trauma Theory Research Practice and Policy, 14(1), 66-79. https://doi.org/10.1037/tra0000913
Uwamaliya, P. (2021). Impact of Initial Health Assessment and Crisis Counselling for Newly Arrived Asylum Seekers. European Psychiatry, 64(S1), S733-S733. https://doi.org/10.1192/j.eurpsy.2021.1942
Youngmann, R., Bachner‐Melman, R., Lev‐Ari, L., Tzur, H., Hileli, R., & Lurie, I. (2021). Trauma, Post-Traumatic Stress Disorder, and Mental Health Care of Asylum Seekers. International journal of environmental research and public health, 18(20), 10661. https://doi.org/10.3390/ijerph182010661