The Effectiveness of Cognitive-Behavioral Therapy on Pain Intensity, Childhood Trauma, Perfectionism, and Psychological Flexibility in Patients with Chronic Pain
Keywords:
Cognitive-behavioral therapy, pain intensity, childhood trauma, perfectionism, psychological flexibility, chronic painAbstract
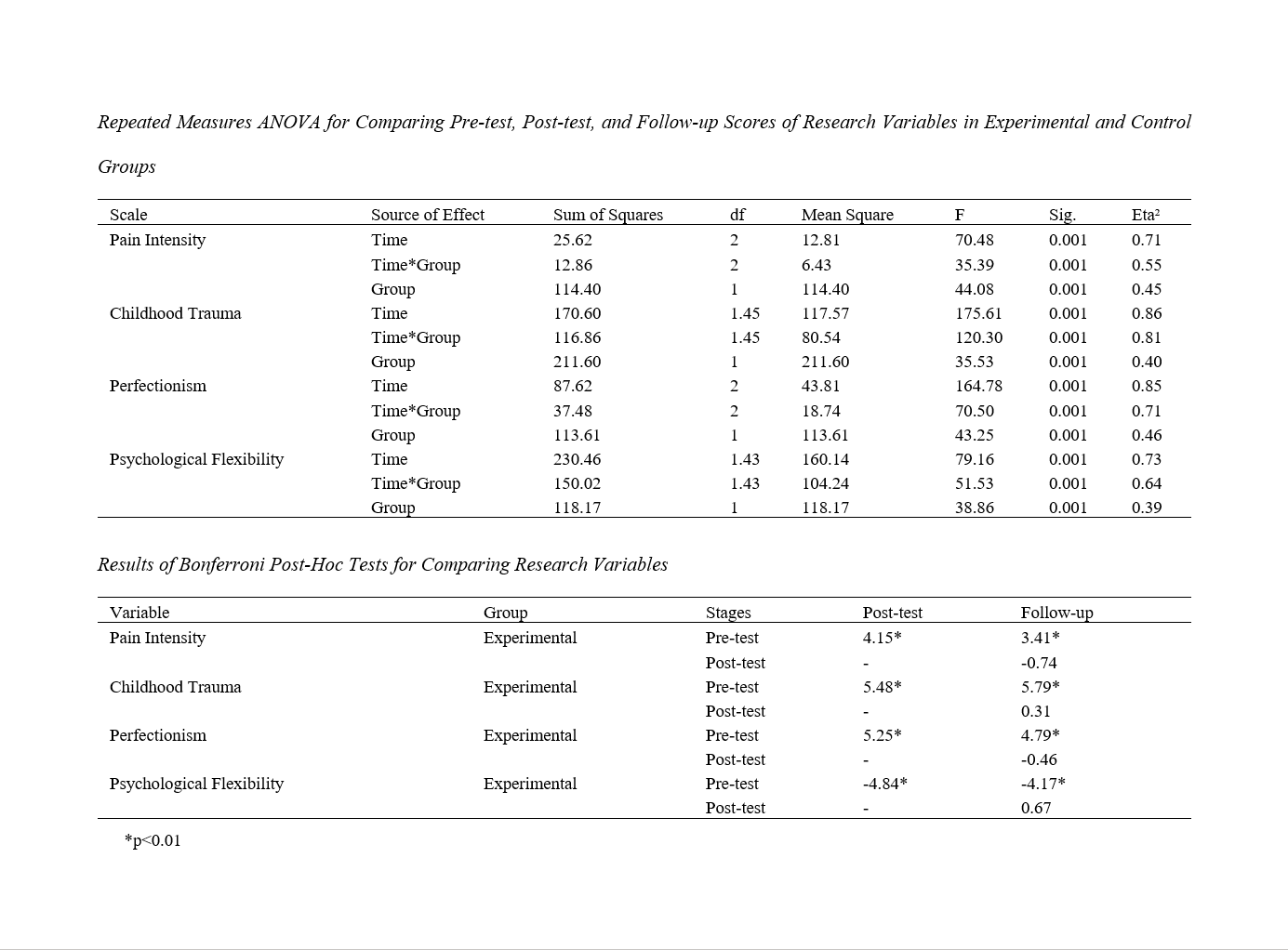
Chronic pain can significantly impact an individual's health status and quality of life, leading to a decrease in health-related quality of life. This study aimed to determine the effectiveness of cognitive-behavioral therapy (CBT) on pain intensity, childhood trauma, perfectionism, and psychological flexibility in patients with chronic pain. This applied and quasi-experimental study employed a pre-test, post-test, and follow-up design with a control group. The statistical population included all chronic pain patients attending pain clinics in Tehran, totaling 198 individuals. From this population, 50 patients were selected through purposive sampling based on inclusion and exclusion criteria and randomly assigned to either the CBT group (25 individuals) or the control group (25 individuals). Data were collected using the West Haven-Yale Multidimensional Pain Inventory (Kerns et al., 1985), the Childhood Trauma Questionnaire (Bernstein et al., 2003), the Multidimensional Perfectionism Scale (Frost et al., 1990), and the Acceptance and Action Questionnaire (Bond et al., 2011). CBT for chronic pain was conducted in seven 60-minute group sessions over two months, based on the treatment package (Kelly Lamb, 2018). Data were analyzed using repeated measures ANOVA with SPSS.22 software. The results indicated that CBT was effective on pain intensity (P<0.001), childhood trauma (P<0.001), perfectionism (P<0.001), and psychological flexibility (P<0.001) in patients with chronic pain. It can be concluded that CBT is effective on pain intensity, childhood trauma, perfectionism, and psychological flexibility in patients with chronic pain. This therapy can be used to reduce the psychological problems of individuals suffering from chronic pain.
Downloads
References
1. McDonagh MS, Morasco BJ, Wagner J, Ahmed AY, Fu R, Kansagara D, et al. Cannabis-Based Products for Chronic Pain. Annals of Internal Medicine. 2022;175(8):1143-53. [PMID: 35667066] [DOI]
2. Groenewald CB, Murray CB, Battaglia M, Scaini S, Quinn PD. Prevalence of Pain Management Techniques Among Adults With Chronic Pain in the United States, 2019. JAMA Network Open. 2022;5(2):e2146697-e. [PMID: 35129599] [PMCID: PMC8822381] [DOI]
3. Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. The Lancet. 2021;397(10289):2082-97. [PMID: 34062143] [DOI]
4. Doorley JD, Goodman FR, Kelso KC, Kashdan TB. Psychological flexibility: What we know, what we do not know, and what we think we know. Social and Personality Psychology Compass. 2020;14(12):e12566. [DOI]
5. Carvalho SA, Trindade IA, Duarte J, Menezes P, Patrão B, Nogueira MR, et al. Efficacy of an ACT and Compassion-Based eHealth Program for Self-Management of Chronic Pain (iACTwithPain): Study Protocol for a Randomized Controlled Trial. Frontiers in Psychology. 2021;12. [PMID: 33767648] [DOI]
6. Goldbart A, Bodner E, Shrira A. The role of emotion covariation and psychological flexibility in coping with chronic physical pain: an integrative model. Psychology & Health. 2021;36(11):1299-313. [PMID: 33136460] [DOI]
7. Coyne LW, Gould ER, Grimaldi M, Wilson KG, Baffuto G, Biglan A. First things first: Parent psychological flexibility and self-compassion during COVID-19. Behavior analysis in practice. 2020:1-7. [DOI]
8. Woodfin V, Hjeltnes A, Binder P-E. Perfectionistic Individuals' Understanding of How Painful Experiences Have Shaped Their Relationship to Others. Frontiers in Psychology. 2021;12. [PMID: 33643148] [PMCID: PMC7905022] [DOI]
9. Alizadeh P, Kooshki S, Tarvirdizadeh H. The Effectiveness of Acceptance and Commitment Therapy and on Pain Intensity, Childhood Trauma, Perfectionism and Psychological Flexibility in Patients with Chronic Pain. Journal of Assessment and Research in Applied Counseling (JARAC). 2023;5(2):123-36. [DOI]
10. Stoeber J, Harvey, Laura N. Multidimensional Sexual Perfectionism and Female Sexual Function: A Longitudinal Investigation. Archives of Sexual Behavior. 2016;45(8):2003-14. [PMID: 27020932] [PMCID: PMC5050246] [DOI]
11. Davey A, Chilcot J, Driscoll E, McCracken LM. Psychological flexibility, self-compassion and daily functioning in chronic pain. Journal of Contextual Behavioral Science. 2020;17:79-85. [DOI]
12. Gilpin HR, Ratanachatchuchai S, Novelli D, McCracken LM, Scott W. Examining the association between group context effects and individual outcomes in an interdisciplinary group-based treatment for chronic pain based on acceptance and commitment therapy. British Journal of Pain. 2022;16(4):420-32. [PMID: 36032341] [PMCID: PMC9411762] [DOI]
13. Goharrizi Zandi G, Ghorban Jahromi, Reza, Robatmili, Somaye, Zare Bahramabadi, Mahdi. Causal Model of Pain Intensity Based on Attachment Styles Mediated by Early Maladaptive Schemas in Patients with Chronic Pain. Psychological Achievements. 2023;30(1):315-32. [DOI]
14. Ahmadi M, Shariat Bagheri MM, Rezaei M, Khazaei S. Predicting the Depression Symptoms by Childhood Traumas in Male Students. Journal of Psychological Studies. 2023;18(4):19-29. [DOI]
15. Karyotaki E, Efthimiou O, Miguel C, Maas genannt Bermpohl F, Furukawa TA, Cuijpers P, et al. Internet-Based Cognitive Behavioral Therapy for Depression: A Systematic Review and Individual Patient Data Network Meta-analysis. JAMA Psychiatry. 2021;78(4):361-71. [PMID: 33471111] [PMCID: PMC8027916] [DOI]
16. Yang Y, Zhang H, Li Y, Liu Z, Liu S, Li X, et al. The effectiveness of computer-assisted Cognitive Behavioral Therapy (cCBT) for psychological outcomes in patients with laryngectomy: Randomized controlled trial. Journal of Affective Disorders. 2022;300:59-65. [PMID: 34942224] [DOI]
17. MacDonald TM, Fisk JD, Bernstein CN, El-Gabalawy R, Hitchon CA, Kornelsen J, et al. The association between childhood maltreatment and pain catastrophizing in individuals with immune-mediated inflammatory diseases. Journal of Psychosomatic Research. 2021;145:110479. [PMID: 33814193] [DOI]
18. González-Robles A, Roca P, Díaz-García A, García-Palacios A, Botella C. Long-term effectiveness and predictors of transdiagnostic internet-delivered cognitive behavioral therapy for emotional disorders in specialized care: secondary analysis of a randomized controlled trial. JMIR mental health. 2022;9(10):e40268. [PMID: 36315227] [PMCID: PMC9664329] [DOI]
19. Bahreini Moghim Jiroft N, Golparvar M, Aghaei A. Comparison of the Effectiveness of Educational Perfectionism Schema Based Strategies Training with Cognitive Behavior Training on Test Anxiety and Academic Burnout among Female Students with Educational Perfectionism. Journal of Educational Psychology Studies. 2023;20(49):20-1. [DOI]
20. Egan SJ, Shafran, Roz. Cognitive-behavioral treatment for perfectionism2017. 284-305 p
21. Golestanibkht T, Babaie E, Masoomzadeh Z. The Effectiveness of Cognitive-Behavioral Therapy on Body Dysmorphic Disorder and Perfectionism Concerns in Students with Physical Deformity Concerns. Journal of Ilam University of Medical Sciences: Volume. 2022;30(6). [DOI]
Downloads
Additional Files
Published
License
Copyright (c) 2024 Parviz Alizadeh (Author); Shirin Kooshki (Corresponding Author); Hajar Tarvirdizadeh (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.