Comparison of the Effectiveness of Self-Care Training and Self-Compassion Training on Hope in Kidney Transplant Patients
Keywords:
Self-care, Self-compassion, Hope, Kidney transplantationAbstract
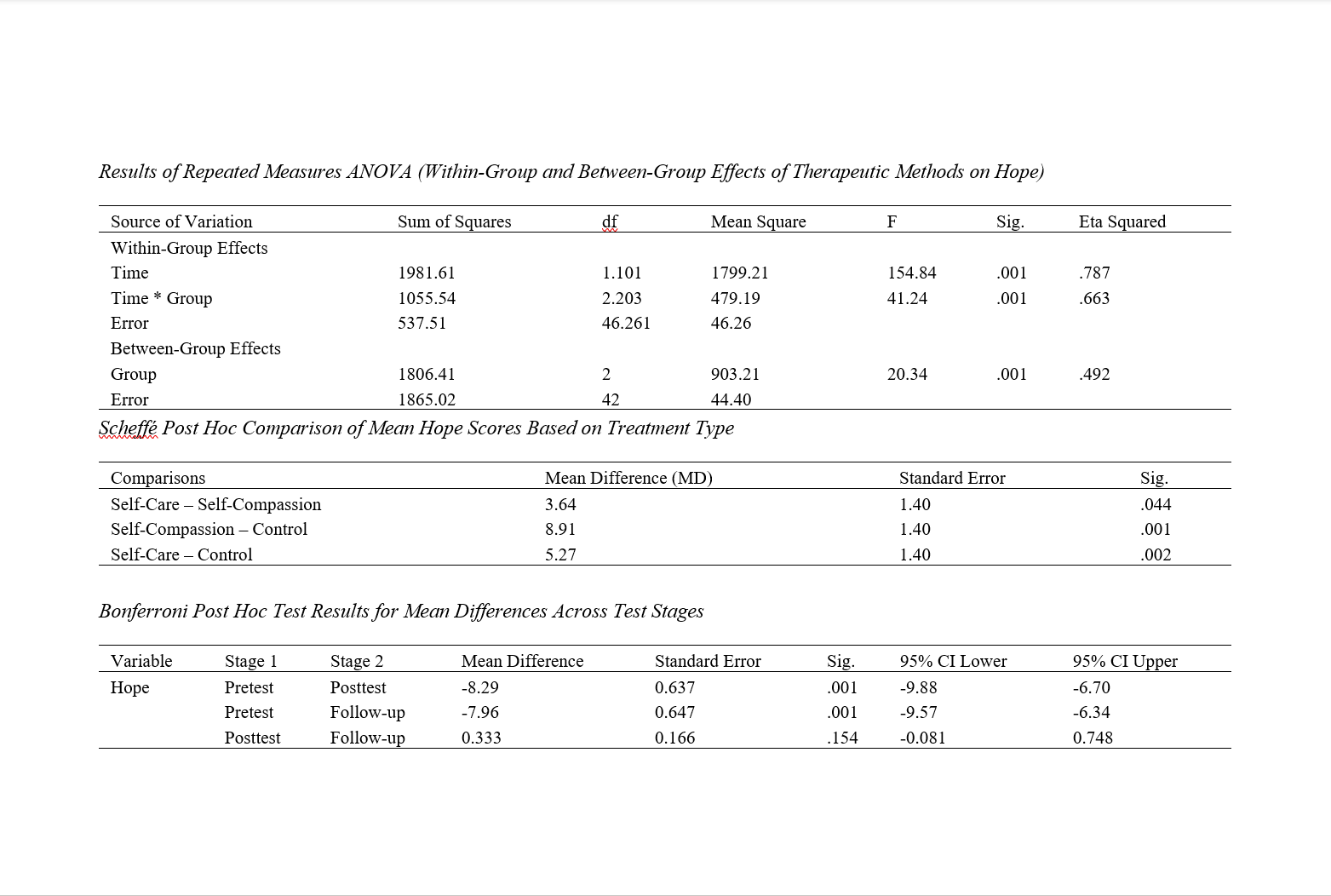
The aim of this study was to compare the effectiveness of self-care training and self-compassion training on hope in kidney transplant patients. The research design was a quasi-experimental pretest-posttest design with a control group and follow-up. The statistical population included all kidney transplant patients who visited Razi Hospital in Rasht during the first quarter of 2024 to consult with urology and dialysis physicians for treatment follow-up. The total number of patients was 176. The study sample consisted of 45 individuals (15 in the self-care group, 15 in the self-compassion group, and 15 in the control group). The instrument used in this study was the Hope Scale by Snyder et al. (1991). The self-care training sessions were conducted in 8 weekly 60-minute sessions, and the self-compassion intervention was administered in 8 weekly 60-minute sessions based on Gilbert’s protocol (2014) in the experimental groups. Repeated measures ANOVA and Bonferroni post-hoc test were used for data analysis. The results indicated that the overall hope scores in both the self-care and self-compassion groups were higher in the posttest and follow-up phases compared to the pretest, in contrast to the control group. Comparison of means showed that self-compassion training was more effective than self-care training in increasing the level of hope. Moreover, a statistically significant difference was found between the self-care group and the control group (p < 0.01), and between the self-compassion group and the control group (p < 0.05), indicating the effectiveness of both self-care and self-compassion training on hope. Overall, it can be concluded that both interventions—self-care and self-compassion—had positive effects on hope, quality of life, and self-confidence in kidney transplant patients. However, differences were observed in the effectiveness of the two interventions. In general, the findings suggest that combining self-care and self-compassion interventions is recommended for achieving optimal outcomes in improving the condition of kidney transplant patients.
Downloads
References
Aburto, J. M., Villavicencio, F., Basellini, U., Kjærgaard, S., & Vaupel, J. W. (2020). Dynamics of life expectancy and life span equality. Proceedings of the National Academy of Sciences, 117(10), 5250-5259. https://doi.org/10.1073/pnas.1915884117
Bai, R., Liu, Y., Zhang, L., Dong, W., Bai, Z., & Zhou, M. (2023). Projections of future life expectancy in China up to 2035: a modelling study. The Lancet Public Health, 8(12), e915-e922. https://doi.org/10.1016/S2468-2667(22)00338-3
Barnett, J. E., & Homany, G. (2022). The new self-care: It's not all about you. Practice Innovations, 7(4), 313. https://doi.org/10.1037/pri0000190
Bedir, M., & Eliüşük-Bülbül, A. (2024). The effect of the self-compassion program on self-compassion and professional quality of life among healthcare professionals. Current Psychology, 43(17), 15376-15384. https://doi.org/10.1007/s12144-023-05516-x
Bilal, U., Hessel, P., Perez-Ferrer, C., Michael, Y. L., Alfaro, T., Tenorio-Mucha, J., Friche, A. A. L., Pina, M. F., Vives, A., Quick, H., Alazraqui, M., Rodriguez, D. A., Miranda, J. J., Diez-Roux, A. V., & group, T. S. (2021). Life expectancy and mortality in 363 cities of Latin America. Nature medicine, 27(3), 463-470. https://doi.org/10.1038/s41591-020-01214-4
Borjali, M., & Naseri Nia, S. (2019). The Effectiveness of Emotion Regulation Strategies Training on Mental Health, Self-compassion and Craving in The Addicts. Counseling Culture and Psycotherapy, 10(40), 133-154. https://qccpc.atu.ac.ir/article_10482.html?lang=en
Bratt, A. S., & Fagerström, C. (2023). Perceptions of General Attitudes towards Older Adults in Society: Is There a Link between Perceived Life Satisfaction, Self-Compassion, and Health-Related Quality of Life? International journal of environmental research and public health, 20(4), 3011. https://doi.org/10.3390/ijerph20043011
Bravo, J. M., Ayuso, M., Holzmann, R., & Palmer, E. (2021). Addressing the life expectancy gap in pension policy. Insurance: Mathematics and Economics, 99, 200-221. https://doi.org/10.1016/j.insmatheco.2021.03.025
Callan, S., Schwartz, J., & Arputhan, A. (2021). Training future psychologists to be competent in self-care: A systematic review. Training and Education in Professional Psychology, 15(2), 117. https://doi.org/10.1037/tep0000345
Chen, Y. C., Chang, L. C., Liu, C. Y., Ho, Y. F., Weng, S. C., & Tsai, T. I. (2018). The Roles of Social Support and Health Literacy in Self-Management Among Patients With Chronic Kidney Disease. Journal of Nursing Scholarship, 50(3), 265-275. https://doi.org/10.1111/jnu.12377
Chuang, L. M., Wu, S. V., Lee, M. C., Lin, L. J., Liang, S. Y., Lai, P. C., & Kao, M. C. (2021). The effects of knowledge and self-management of patients with early-stage chronic kidney disease: Self-efficacy is a mediator. Japan Journal of Nursing Science, 18(2), e12388. https://doi.org/10.1111/jjns.12388
Chukwuorji, J. C., Odi, C. P., Chike-Okoli, A., Morah, N. M., Osondu, O. M., Rukmi, D. K., Victor-Aigbodion, V., & Eze, J. E. (2024). Health-related quality of life of people living with HIV: contributions of emotion regulation and self-compassion. Venereology, 3(3), 136-146. https://doi.org/10.3390/venereology3030011
Costa, D. S., Mercieca-Bebber, R., Rutherford, C., Tait, M. A., & King, M. T. (2021). How is quality of life defined and assessed in published research? Quality of Life Research, 30, 2109-2121. https://doi.org/10.1007/s11136-021-02826-0
Dabuke, A. M., Zainal, V. R., & Hakim, A. (2023). The Effect of Self-Ability and Self Confidence on Employee Performance: A Literature Review. Dinasti International Journal of Digital Business Management, 4(2), 286-296. https://dinastipub.org/DIJDBM/article/view/1704
Hashemi, Z., Aghajani Heshjin, T., & Shokrgozar, A. (2024). The Relationship Between Spiritual Well-being, Mental Health, Resilience, and Hope in Cardiovascular Patients. Research in Religion and Health, 8(Fall 2021), 38-52. http://ensani.ir/fa/article/509232/%D8%B1%D8%A7%D8%A8%D8%B7%D9%87-%D8%A8%D9%87%D8%B2%DB%8C%D8%B3%D8%AA%DB%8C-%D9%85%D8%B9%D9%86%D9%88%DB%8C-%D8%A8%D8%A7-%D8%B3%D9%84%D8%A7%D9%85%D8%AA-%D8%B1%D9%88%D8%A7%D9%86-%D8%AA%D8%A7%D8%A8-%D8%A2%D9%88%D8%B1%DB%8C-%D9%88-%D8%A7%D9%85%DB%8C%D8%AF-%D8%A8%D9%87-%D8%B2%D9%86%D8%AF%DA%AF%DB%8C-%D8%AF%D8%B1-%D8%A8%DB%8C%D9%85%D8%A7%D8%B1%D8%A7%D9%86-%D9%82%D9%84%D8%A8%DB%8C-%D8%B9%D8%B1%D9%88%D9%82%DB%8C-%D8%A8%DB%8C%D9%85%D8%A7%D8%B1%D8%B3%D8%AA%D8%A7%D9%86-%D8%AC%D9%85-%D8%B4%D9%87%D8%B1-%D8%AA%D9%87%D8%B1%D8%A7%D9%86
Sharifian, P. (2024). Effect of Resilience Training on Stress, Hope and Psychological Toughness of Mothers Living With Mentally and Physically Disabled Children. BMC pediatrics, 24(1). https://doi.org/10.1186/s12887-024-04828-6
Downloads
Additional Files
Published
Submitted
Revised
Accepted
License
Copyright (c) 2025 Maryam Saeidi (Author); Mohammadreza Zarbakhsh Bahri (Corresponding Author); Ali khaneh Keshi (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.