Voices of Recovery: Patients’ Experiences with AI-Assisted Stroke Rehabilitation
Keywords:
AI-assisted rehabilitation, stroke recovery, patient experience, human–technology interaction, qualitative study, neurorehabilitationAbstract
Objective: This study aims to explore the lived experiences of stroke survivors engaging in AI-assisted rehabilitation.
Methods and Materials: This qualitative study was conducted with 14 stroke survivors undergoing AI-assisted rehabilitation at the York Rehab Center in Richmond Hill, Canada. Participants were recruited using purposive sampling, and data collection was carried out through in-depth, semi-structured interviews. Interviews lasted 45–60 minutes and were audio-recorded, transcribed verbatim, and coded using NVivo 14 software. Thematic analysis was employed following Braun and Clarke’s six-phase framework. The study continued until theoretical saturation was achieved. Ethical considerations including informed consent and confidentiality were rigorously maintained throughout the research process.
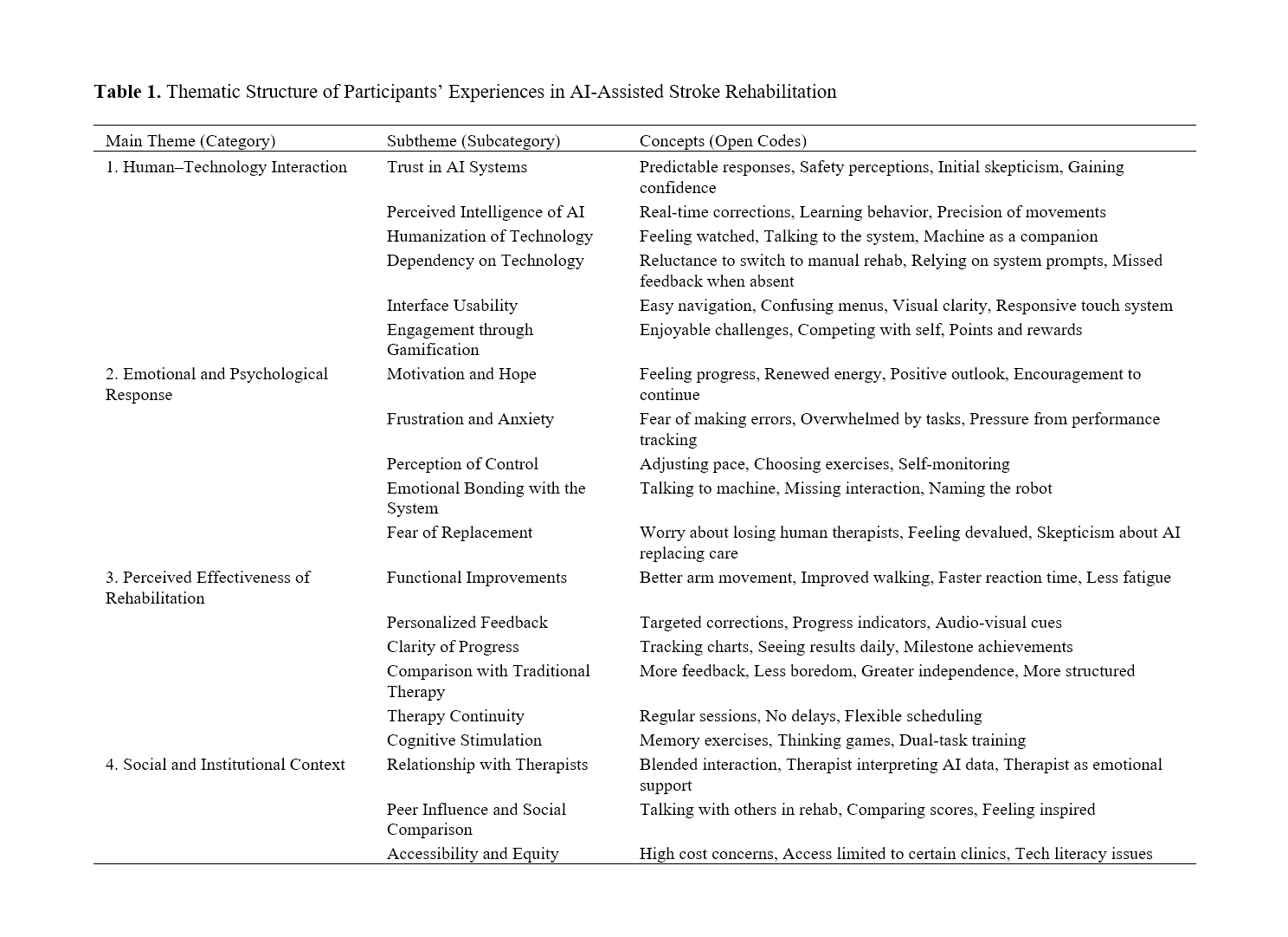
Findings: Analysis revealed four main themes: (1) Human–Technology Interaction, including trust in AI and interface usability; (2) Emotional and Psychological Response, encompassing motivation, emotional bonding with technology, and performance anxiety; (3) Perceived Effectiveness of Rehabilitation, including functional improvement, personalized feedback, and therapy comparison; and (4) Social and Institutional Context, focusing on relationships with therapists, digital equity, and cultural influences. Patients generally found the AI systems to be engaging and supportive of their physical recovery. However, emotional detachment, dependence, and accessibility challenges emerged as concerns. Participants emphasized the need for human involvement alongside AI systems to ensure emotional and motivational support.
Conclusion: AI-assisted rehabilitation was perceived as a promising and effective complement to traditional therapy, enhancing functional outcomes and patient engagement. However, its full potential lies in hybrid models that integrate human empathy with technological precision.
Downloads
References
1. Zou Z. Design and Interaction Optimization of Smart Hand Rehabilitation Assistive Devices for Stroke Patients. Computer Fraud & Security. 2025:1258-66.
2. Singh A. From Mind to Motion: The Promise of Brain Computer Interfaces and Myoelectric Prosthetics for Stroke Neurorehabilitation. Interantional Journal of Scientific Research in Engineering and Management. 2025;09(02):1-9.
3. Kishor I, Goyal P, Gantla HR, Goyal P, Mamodiya U. AI-Driven Haptic Technologies Revolutionizing Patient Rehabilitation. 2025:47-84.
4. Baysal Z. AI-Driven Rehabilitation Robots: Enhancing Physical Therapy for Stroke and Injury Recovery. Nflsai. 2024;8(1):155.
5. Hao M, Wang X, Tao W, Sheng C. Repetitive Transcranial Magnetic Stimulation Combined With Ginkgo Diterpene Lactone Meglumine Injection Recover Cognitive and Neurological Functions of Patients With Acute Ischemic Stroke. Actas Esp Psiquiatr. 2025;53(1):110-8.
6. Reis TC, Machado A. Advancing Post‐Stroke Rehabilitation: Emerging and Current Neuromodulation Approaches and Integration of Artificial Intelligence‐Driven Closed‐Loop Systems. Sensory Neuroscience. 2025;1(1).
7. Ono K, Takahashi R, Morita K, Ara Y, Abe S, Ito S, et al. Can AI Predict Walking Independence in Patients With Stroke Upon Admission to a Recovery-Phase Rehabilitation Ward? Japanese Journal of Comprehensive Rehabilitation Science. 2024;15(0):1-7.
8. Hsiao C-C, Cheng C-G, Chen C-C, Chiu HW, Lin HC, Cheng CA. Semantic Visualization in Functional Recovery Prediction of Intravenous Thrombolysis Following Acute Ischemic Stroke in Patients by Using Biostatistics: An Exploratory Study. Journal of Personalized Medicine. 2023;13(4):624.
9. Wong LH, Aw GP, Sun H, Yen CC, Teo CG, Wen Y. Effects of a Machine Learning-Empowered Chinese Character Handwriting Learning Tool on Rectifying Legible Writing in Young Children: A Pilot Study. Icce. 2023.
10. Tran LV, Alvarez XA, Le H-A, Nguyen D-A, Le TN, Nguyen PN, et al. Clinical Efficacy of Cerebrolysin and Cerebrolysin Plus Nootropics in the Treatment of Patients With Acute Ischemic Stroke in Vietnam. CNS & Neurological Disorders - Drug Targets. 2022;21(7):621-30.
11. Paul T, Wiemer VM, Günther J, Lehnberg FM, Grafton ST, Fink GR, et al. Reward Enhances Motor Adaptation Learning in Acute Stroke Patients. 2024.
12. Zhang Y, Luo X, Song X, Li J, Liu Y, Wang L, et al. Efficacy of Human Urinary Kallidinogenase in Real-World Patients With Acute Ischemic Stroke. The Neurologist. 2025.
13. Zhang Y, Zhou F, Li H, Lei J, Mo Z, Li G, et al. Efficacy and Safety of Dl-3-N-Butylphthalide Combined With Human Urinary Kallidinogenase in the Treatment of Acute Ischemic Stroke. Clinical Neuropharmacology. 2023;46(2):60-5.
14. Chen J, Gao X, Liang J, Wu Q, Shen L, Zheng Y, et al. Association Between Gut Microbiota Dysbiosis and Poor Functional Outcomes in Acute Ischemic Stroke Patients With COVID-19 Infection. Msystems. 2024;9(6).
15. Lu J, Zhang L, Zhang Y, Mao H, Fang Q. Intravenous Thrombolysis and Risk of Early-Onset Post-Stroke Depression: A Propensity Score Matched Cohort Study. Frontiers in Neurology. 2024;15.
16. Li Z, Pang M, Yu Y, Peng T, Hu Z, Niu R, et al. Effect of Different Ventilation Modalities on the Early Prognosis of Patients With Sleep Apnea After Acute Ischemic Stroke–––protocol for a Prospective, Open-Label and Randomised Controlled Trial. BMC Neurology. 2023;23(1).
17. Jiang R, Lai Y-T. Predictive Role of Neuron-Specific Enolase and S100-Β in Early Neurological Deterioration and Unfavorable Prognosis in Patients With Ischemic Stroke. Open Medicine. 2024;19(1).
18. Couture L, Cahuiche AE, Petway A, Baskin LS, Colpo GD, McCullough LD. Abstract 422: The Impact of Household Composition on Acute Ischemic Strokes: Acute and Chronic Implications. Stroke Vascular and Interventional Neurology. 2024;4(S1).
19. Taleb S, Lee JJ, Duncan PW, Cramer SC, Hosseini MB, Su M, et al. Essential Information for Neurorecovery Clinical Trial Design: Trajectory of Global Disability in First 90 Days post-Stroke in Patients Discharged to Acute Rehabilitation Facilities. BMC Neurology. 2023;23(1).
20. Sablić S, Dolić K, Kraljević I, Budimir D, Čičmir-Vestić M, Benzon B, et al. The Presence of Communicating Arteries in the Circle of Willis Is Associated With Higher Rate of Functional Recovery After Anterior Circulation Ischemic Stroke. Biomedicines. 2023;11(11):3008.
21. Bonkhoff AK, Schirmer MD, Bretzner M, Etherton MR, Donahue K, Tuozzo C, et al. Abnormal Dynamic Functional Connectivity Is Linked to Recovery After Acute Ischemic Stroke. Human Brain Mapping. 2021;42(7):2278-91.
22. Taleb S, Lee JJ, Duncan PW, Cramer SC, Hosseini MB, Su M, et al. Essential Information for Neurorecovery Clinical Trial Design: Trajectory of Global Disability in First 90 Days Poststroke in Patients Discharged to Acute Rehabilitation Facilities. 2022.
23. Gao J, Shao X, Guan Y, Mei J. Effect of Danhong Injection on Neurological Recovery and Adverse Events in Patients With Acute Ischemic Stroke. Medicine. 2021;100(46):e27683.
24. Li Y, Wang W, Yang H, Guo W, Feng J, Yang D, et al. Negative Correlation Between Early Recovery and Lipoprotein-Associated Phospholipase A2 Levels After Intravenous Thrombolysis. Journal of International Medical Research. 2022;50(4).
25. Kaur D. A Comparative Analysis of Diagnostic Imaging in Acute Ischaemic Stroke. Chettinad Health City Medical Journal. 2023;12(02):3-8.
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2025 James Ma, Seyed Alireza Saadati (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.