Relationship between Laryngeal Disorders and Respiratory Function in Professional Road Cyclists
Keywords:
Laryngeal Disorders, Road Cyclists, Outdoor Exercise, Respiratory FunctionAbstract
Objective: Engaging in outdoor cycling, particularly within cold and arid environments, frequently precipitates dryness in the laryngeal mucosa and induces various supraglottic disorders. Such conditions hold the potential to detrimentally impact respiratory system efficiency. This study principally sought to elucidate the influence of supraglottic and upper airway disorders on the respiratory capacities of road cyclist.
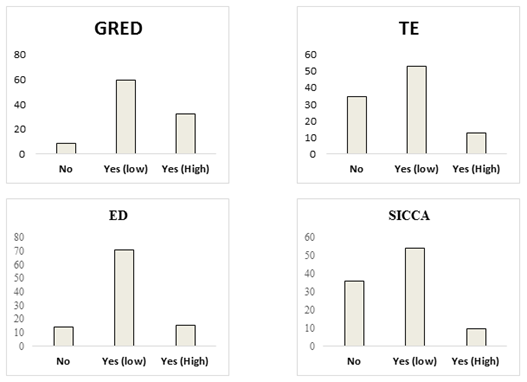
Methods and Materials: This investigation encompassed seventy-two professional and elite road cyclists, comprising 22 females and 50 males, with an average age of 22 years and a Body Mass Index (BMI) of 21.95(±0.02) kg/m². Utilizing stroboscopic examinations, supraglottic conditions including Sicca, Tension, Edema, and Gastroesophageal Reflux Disease were assessed. Concurrently, respiratory capacity was evaluated through spirometric tests, encompassing Forced Vital Capacity [FVC], Forced Expiratory Volume in the first second [FEV1], Tidal Volume [VT], Maximum Vital Capacity [VC MAX], Mean Mid-Expiratory Flow [MMEF (FEF25-75)], Peak Expiratory Flow [PEF], and Controlled Mechanical Volume Ventilation [cMVV]. Analysis of Variance (ANOVA) was employed to analyze the relationship between stroboscopic and spirometric findings, additionally exploring correlations between the two. A backward method in regression analysis was used, with Edema (ED), Gastroesophageal Reflux Disease (GERD), Dry Laryngeal Mucosa (Sicca), and Tension (TE) serving as predictor variables against spirometric outcomes.
Results: Predominantly, participants exhibited low levels of ED, GERD, Sicca, and TE. No substantial correlation emerged between ED, GERD, TE, and any spirometric indices (p-value > 0.05). However, a notable relationship was observed between Sicca and the MMEF index (p-value < 0.05). Regression analysis revealed significant outcomes for independent variables impacting VT and MEF25, with GERD negatively influencing VT in a statistically significant manner. Likewise, GERD's effect on the MEF25 variable was both negative and significant.
Conclusion: This research offers critical insights into the impact of adverse training conditions and laryngeal disorders on respiratory function in cyclists. Addressing these concerns could facilitate considerable enhancements in their performance during training and competitive events.
Downloads
References
1. Hamdan AL, Sataloff RT, Hawkshaw M. Voice
Disorders in Athletes, Coaches and Other Sports Professionals:
Springer; 2021. [DOI]
2. Xu W. Atlas of Strobolaryngoscopy: Springer; 2019.
[DOI]
3. Peroš-Golubičić T, Tekavec-Trkanjec J. Upper
respiratory tract infections. Textbook of Respiratory and Critical
Care Infections. 2015;1:16. [DOI]
4. Rouev P, Chakarski I, Doskov D, Dimov G, Staykova E.
Laryngopharyngeal symptoms and gastroesophageal reflux
disease. Journal of Voice. 2005;19(3):476-80. [PMID: 15936924]
[DOI]
5. Boulet L-P, Turmel J. Cough in exercise and athletes.
Pulmonary pharmacology & therapeutics. 2019;55:67-74. [PMID:
22487846] [PMCID: PMC3580050] [DOI]
6. Kolnes L-J, Vollsæter M, Røksund OD, Stensrud T.
Physiotherapy improves symptoms of exercise-induced laryngeal
obstruction in young elite athletes: a case series. BMJ open sport &
exercise medicine. 2019;5(1):e000487. [PMID: 30740235]
[PMCID: PMC6347884] [DOI]
7. Jozkow P, Wasko-Czopnik D, Medras M, Paradowski L.
Gastroesophageal reflux disease and physical activity. Sports
medicine. 2006;36(5):385-91. [PMID: 16646627] [DOI]
8. de Oliveira EP, Burini RC, Jeukendrup A.
Gastrointestinal complaints during exercise: prevalence, etiology,
and nutritional recommendations. Sports Medicine. 2014;44(1):79-
85. [PMID: 24791919] [PMCID: PMC4008808] [DOI]
9. Parmelee-Peters K, Moeller JL. Gastroesophageal reflux
in athletes. Current sports medicine reports. 2004;3(2):107-11.
[PMID: 14980140] [DOI]
10. Ostapiak Z, Vypasniak I, Lisovskyi B, Mytskan T.
Respiratory Tract Dysfunction in Sportsmen. Physical education,
sport and health culture in modern society. 2017(2 (38)):169-77.
[DOI]
11. Sodhi JS, Zargar SA, Javid G, Khan MA, Khan BA,
Yattoo G, et al. Effect of bending exercise on gastroesophageal
reflux in symptomatic patients. Indian J Gastroenterol.
2008;27(6):227-31.
12. Hamdan A-L, Sataloff RT, Hawkshaw MJ. ExerciseInduced Laryngeal Obstruction (EILO) in Athletes. Voice
Disorders in Athletes, Coaches and other Sports Professionals:
Springer; 2021. p. 155-82. [DOI]
13. Kolnes L-J, Stensrud T. Exercise-induced laryngeal
obstruction in athletes: contributory factors and treatment
implications. Physiotherapy theory and practice.
2019;35(12):1170-81. [PMID: 29757061] [DOI]
14. Fan E, Olin JT. Exercise-induced laryngeal obstruction.
American journal of respiratory and critical care medicine.
2019;199(12):P23-P4. [PMID: 31199188] [DOI]
15. Prontenko K, Griban G, Prontenko V, Bezpaliy S,
Bykova G, Dvoretsky V. Level and dynamics of functional
preparedness indexes of kettlebell sportsmen. Journal of Physical
Education and Sport. 2017(17):712-6.
16. Castro M, Dedivitis RA, Macedo AG. Evaluation of a
method for assessing pulmonary function in laryngectomees. Acta
Otorhinolaryngologica Italica. 2011;31(4):243.
17. Koyunlu A, Dağlioğlu Ö, Özdal M. Comparison of
Physical Fitness and Respiratory Parameters of Elite Wrestlers and
Judokas. Turkish Journal of Sport and Exercise. 2020;22(3):360-5.
18. Al-Alwan A, Kaminsky D. Vocal cord dysfunction in
athletes: clinical presentation and review of the literature. The
Physician and sportsmedicine. 2012 May 1;40(2):22-7. [PMID:
22759602] [DOI]
19. Baz M, Haji G, Menzies-Gow A, Tanner R, Hopkinson
N, Polkey M, Hull J. Dynamic laryngeal narrowing during exercise:
a mechanism for generating intrinsic PEEP in COPD? Thorax.
2015;70(3):251-7. [PMID: 25586938] [PMCID: PMC4345987]
[DOI]
20. Sivasankar M, Fisher KV. Oral breathing increases Pth
and vocal effort by superficial drying of vocal fold mucosa. Journal
of Voice. 2002;16(2):172-81. [PMID: 12150370] [DOI]
21. Nielsen EW, Hull JH, Backer V. High prevalence of
exercise-induced laryngeal obstruction in athletes. Medicine and
science in sports and exercise. 2013;45(11):2030-5. [PMID:
23657163] [DOI]
22. Sandnes A, Hilland M, Clemm HH, Heimdal J-H,
Halvorsen T, Røksund OD. Laryngoscopy but not resting
spirometry is diagnostic for exercise induced laryngeal obstruction.
Eur Respiratory Soc; 2013.
23. Fretzayas A, Moustaki M, Loukou I, Douros K.
Differentiating vocal cord dysfunction from asthma. Journal of
asthma and allergy. 2017;10:277. [PMID: 29066919] [PMCID:
PMC5644529] [DOI]
24. Walsted ES, Swanton LL, van van Someren K, Morris
TE, Furber M, Backer V, Hull JH. Laryngoscopy during
swimming: a novel diagnostic technique to characterize swimming‐
induced laryngeal obstruction. The Laryngoscope.
2017;127(10):2298-301. [PMID: 28236311] [DOI]
25. Colbey C, Cox AJ, Pyne DB, Zhang P, Cripps AW, West
NP. Upper respiratory symptoms, gut health and mucosal immunity
in athletes. Sports Medicine. 2018;48(1):65-77. [PMID: 29363055]
[PMCID: PMC5790851] [DOI]
26. Dickinson JW, Greenwell J, Hull JH. Epilogue: Bringing
it all together to optimise athlete respiratory care. Complete Guide
to Respiratory Care in Athletes: Routledge; 2020. p. 182-96. [DOI]
27. Sandnes A, Andersen T, Clemm HH, Hilland M,
Heimdal J-H, Halvorsen T, et al. Clinical responses following
inspiratory muscle training in exercise-induced laryngeal
obstruction. European Archives of Oto-Rhino-Laryngology.
2022;279(5):2511-22. [PMID: 34954812] [PMCID:
PMC8986676] [DOI]
28. Clemm HH, Olin JT, McIntosh C, Schwellnus M, Sewry
N, Hull JH, Halvorsen T. Exercise-induced laryngeal obstruction
(EILO) in athletes: a narrative review by a subgroup of the IOC
Consensus on ‘acute respiratory illness in the athlete’. British
Journal of Sports Medicine. 2022;56(11):622-9. [PMID:
35193856] [PMCID: PMC9120388] [DOI]
29. Ebrahimi S, Gholami MJJoV. Comparison of Maximum
Oxygen Uptake and Rating Perceived Exertion in Woman's
Kabaddi Athletes (Without Breathy Voice to Severe Breathy
Voice). 2018.
30. Hankinson JL, Odencrantz JR, Fedan KBJAjor, medicine
cc. Spirometric reference values from a sample of the general US
population. 1999;159(1):179-87. [PMID: 9872837] [DOI]
31. Alemayehu HK, Salvadego D, Tringali G, De Micheli R,
Caccavale M, Sartorio A, Grassi BJSR. Acute respiratory muscle
unloading improves time-to-exhaustion during moderate-and
heavy-intensity cycling in obese adolescent males. 2020;10(1):1-9.
[PMID: 33046823] [PMCID: PMC7550339] [DOI]
32. Casper JK, Leonard R. Understanding voice problems: A
physiological perspective for diagnosis and treatment: Lippincott
Williams & Wilkins; 2006.
33. Won H-K, Kang S-Y, Kang Y, An J, Lee J-H, Lee SM,
et al. Cough-related laryngeal sensations and triggers in adults with
chronic cough: symptom profile and impact. 2019;11(5):622.
[PMID: 31332974] [PMCID: PMC6658400] [DOI]
34. Dou ZJE. Effects of Atmospheric Particulate Matter
Pollution on Physical Function of Elderly Sports Population.
2019;28(108):2057-62.
35. Sue‐Chu M, Kippelen PJCLF. Effects of Cold and Heat
on the Lung. 2020:653-9. [DOI]
36. Fretzayas A, Moustaki M, Loukou I, Douros KJJoa,
allergy. Differentiating vocal cord dysfunction from asthma.
2017;10:277. [PMID: 29066919] [PMCID: PMC5644529] [DOI]
37. Dickinson JW, Boniface A. Breathing pattern disorders
in athletes. Complete Guide to Respiratory Care in Athletes:
Routledge; 2020. p. 147-69. [DOI]
38. Marcinow AM, Thompson J, Chiang T, Forrest LA,
deSilva BWJTL. Paradoxical vocal fold motion disorder in the elite
athlete: experience at a large division I university.
2014;124(6):1425-30. [PMID: 24166723] [DOI]
39. Sivasankar M, Fisher KVJJoV. Oral breathing increases
Pth and vocal effort by superficial drying of vocal fold mucosa.
2002;16(2):172-81. [PMID: 12150370] [DOI]
40. Forrest LA, Husein T, Husein O. Paradoxical vocal cord
motion: classification and treatment. The Laryngoscope.
2012;122(4):844-53. [PMID: 22434681] [DOI]
41. Fairfax A, Haslam P, Pavir D, Sheahan N, Bateman J,
Agnew J, et al. Pulmonary disorders associated with Sjögren's
syndrome. QJM: An International Journal of Medicine.
1981;50(3):279-95.
42. Pirogowicz I, Patyk M, Popecki P, Rudnicki J, Gojny L,
Pokorski M. Lung function in patients with gastro-esophageal
reflux disease and respiratory symptoms. Neurobiology of
Respiration. 2013:161-6. [PMID: 23835974] [DOI]
43. Theodoropoulos DS, Pecoraro DL, Efstratiadis SE. The
association of gastroesophageal reflux disease with asthma and
chronic cough in the adult. American Journal of Respiratory
Medicine. 2002;1:133-46. [PMID: 14720067] [DOI]
44. Sundar KM, Stark A, Morris MJ. Laryngeal Dysfunction
Manifesting as Chronic Refractory Cough and Dyspnea Laryngeal
Physiology in Respiratory Health and Disease. Chest. 2024.
[PMID: 38508333] [DOI]
45. Green SB. How many subjects does it take to do a
regression analysis. Multivariate behavioral research.
1991;26(3):499-510. [PMID: 26776715] [DOI]
Downloads
Additional Files
Published
Submitted
Revised
Accepted
Issue
Section
License
Copyright (c) 2024 Samaneh Ebrahimi, Khadijeh Irandoust, Samira Sadat Ghalishourani, Mandana Gholami, Mohsen Avatef Rostami, Aslan Ahmadi (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.