The Effectiveness of Acceptance and Commitment Therapy on Psychological Well-being, Resilience, and Hope for Life in Coronary Heart Disease Patients with High Blood Pressure Visiting Shahid Rajaei Hospital
Keywords:
Hope for life, Resilience, Psychological well-being, Coronary heart disease patients, Acceptance and Commitment TherapyAbstract
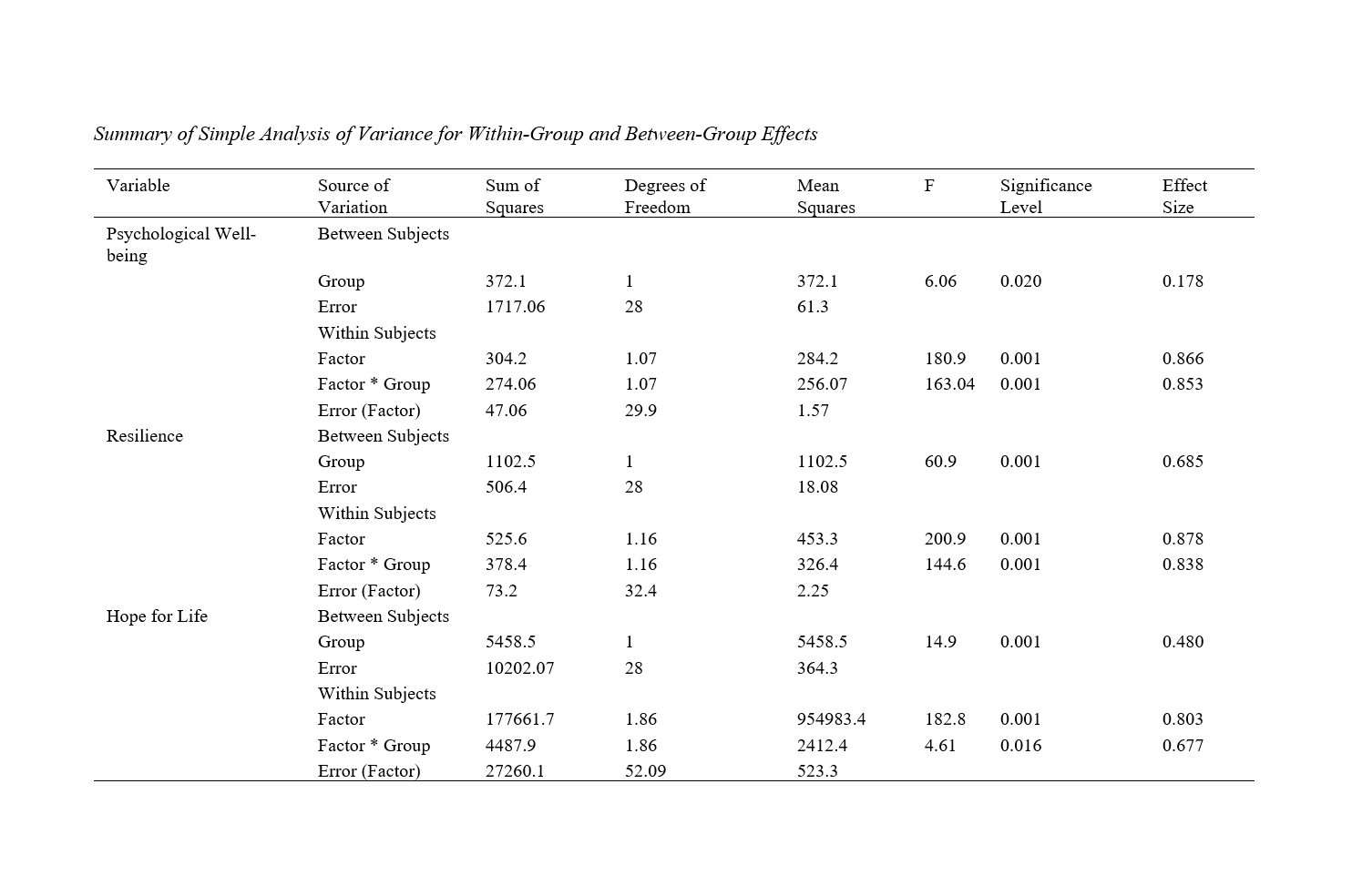
The purpose of this study was to examine the effectiveness of Acceptance and Commitment Therapy (ACT) on psychological well-being, resilience, and hope for life among patients with coronary heart disease and high blood pressure who attended Shahid Rajaei Hospital. This was a quasi-experimental study with a pre-test, post-test, and a 3-month follow-up, including a control group. The study population included all individuals with a diagnosis of coronary heart disease and high blood pressure. The sample consisted of 30 patients selected through purposive sampling and randomly assigned to either the experimental or the control group. Data were collected using Ryff's Psychological Well-being Scale (1989), Bond et al.'s Resilience Scale (2011), and Snyder et al.'s Life Hope Scale (1991). The ACT intervention was conducted over eight 90-minute sessions held weekly; however, the control group received no intervention. Data analysis was performed using a repeated measures analysis of variance (ANOVA) with SPSS-26. Findings indicated that Acceptance and Commitment Therapy significantly enhances psychological well-being, resilience, and hope for life in patients with coronary heart disease and high blood pressure (p < 0.05). In conclusion, ACT can improve psychological well-being, resilience, and life expectancy in patients with coronary heart disease and high blood pressure. Therefore, this approach can be used alongside medical interventions in healthcare centers.
Downloads
References
1. Jamil Y, Park DY, Verde LM, Sherwood MW, Tehrani BN, Batchelor WB, et al. Do Clinical Outcomes and Quality of Life Differ by the Number of Antianginals for Stable Ischemic Heart Disease? Insights from the BARI 2D Trial. American Journal of Cardiology. 2024;214:66-76. [PMID: 38160927] [DOI]
2. Afshinpoor F, Khorami NS, Nabavi SA. The effectiveness of acceptance and commitment therapy on anxiety and quality of life in patients with non-cardiac chest pain. shenakht Journal of Psychology and Psychiatry. 2021;8(5):56-68. [DOI]
3. Scharbert J, Humberg S, Kroencke L, Reiter T, Sakel S, ter Horst J, et al. Psychological well-being in Europe after the outbreak of war in Ukraine. Nature Communications. 2024;15(1):1202. [PMID: 38378761] [PMCID: PMC10879508] [DOI]
4. Rubino F, Pompei G, Brugaletta S, Collet C, Kunadian V. The role of physiology in the contemporary management of coronary artery disease. Heart. 2024;110(6):391-8. [PMID: 37827561] [DOI]
5. Xie Q, Nie M, Zhang F, Shao X, Wang J, Song J, Wang Y. An unexpected interaction between diabetes and cardiovascular diseases on cognitive function: A cross-sectional study. Journal of Affective Disorders. 2024;354:688-93. [PMID: 38521139] [DOI]
6. Gulati M, Khan N, George M, Berry C, Chieffo A, Camici PG, et al. Ischemia with no obstructive coronary artery disease (INOCA): A patient self-report quality of life survey from INOCA international. International Journal of Cardiology. 2023;371:28-39. [PMID: 36162521] [DOI]
7. Trajković N, Mitić PM, Barić R, Bogataj Š. Effects of physical activity on psychological well-being. Frontiers in psychology. 2023;14:1121976. [PMID: 36743250] [PMCID: PMC9890147] [DOI]
8. Shang Y, Nasr P, Widman L, Hagström H. Risk of cardiovascular disease and loss in life expectancy in NAFLD. Hepatology. 2022;76(5). [PMID: 35403232] [PMCID: :PMC9790251] [DOI]
9. Cole L, Ridings L, Phillips SM. Stress and Coping Factors Affecting Health-Related Quality of Life in Parents of Children with Congenital Heart Disease: An Integrative Review. Pediatric Cardiology. 2024;45(3):457-70. [PMID: 37466733] [DOI]
10. Guo L, Chen J, Yuan W. The effect of HIIT on body composition, cardiovascular fitness, psychological well-being, and executive function of overweight/obese female young adults. Frontiers in Psychology. 2023;13. [PMID: 36743598] [PMCID: PMC9891140] [DOI]
11. Jyotsna FNU, Ahmed A, Kumar K, Kaur P, Chaudhary MH, Kumar S, et al. Exploring the Complex Connection Between Diabetes and Cardiovascular Disease: Analyzing Approaches to Mitigate Cardiovascular Risk in Patients With Diabetes. Cureus. 2023;15(8):e43882. [DOI]
12. Fan Y, Ho M-HR, Shen B-J. Loneliness predicts physical and mental health-related quality of life over 9 months among patients with coronary heart disease. Applied Psychology: Health and Well-Being. 2023;15(1):152-71. [PMID: 36184794] [DOI]
13. Iida H, Fujimoto S, Wakita T, Yanagi M, Suzuki T, Koitabashi K, et al. Psychological flexibility and depression in advanced CKD and dialysis. Kidney medicine. 2020;2(6):684-91. e1. [PMID: 33319193] [PMCID: PMC7729231] [DOI]
14. Edwards DJ, Pinna T. A Systematic Review of Associations Between Interoception, Vagal Tone, and Emotional Regulation: Potential Applications for Mental Health, Wellbeing, Psychological Flexibility, and Chronic Conditions. Frontiers in Psychology. 2020;11. [PMID: 32849058] [PMCID: PMC7419655] [DOI]
15. Huang B-H, del Pozo Cruz B, Teixeira-Pinto A, Cistulli PA, Stamatakis E. Influence of poor sleep on cardiovascular disease-free life expectancy: a multi-resource-based population cohort study. BMC Medicine. 2023;21(1):75. [PMID: 36859313] [PMCID: PMC9979412] [DOI]
16. Wielgus B, Urban W, Patriak A, Cichocki Ł. Examining the Associations between Psychological Flexibility, Mindfulness, Psychosomatic Functioning, and Anxiety during the COVID-19 Pandemic: A Path Analysis. International Journal of Environmental Research and Public Health. 2020;17(23):8764. [PMID: 33255758] [PMCID: PMC7728363] [DOI]
17. Landi G, Pakenham KI, Benassi M, Giovagnoli S, Tossani E, Grandi S. A Model of the Effects of Parental Illness on Youth Adjustment and Family Functioning: The Moderating Effects of Psychological Flexibility on Youth Caregiving and Stress. International Journal of Environmental Research and Public Health. 2021;18(9):4902. [PMID: 34064517] [PMCID: PMC8124913] [DOI]
18. Edwards DJ, Lowe R. Associations Between Mental Health, Interoception, Psychological Flexibility, and Self-as-Context, as Predictors for Alexithymia: A Deep Artificial Neural Network Approach. Frontiers in Psychology. 2021;12. [PMID: 33868110] [PMCID: PMC8044902] [DOI]
19. Frinking E, Jans-Beken L, Janssens M, Peeters S, Lataster J, Jacobs N, Reijnders J. Gratitude and loneliness in adults over 40 years: examining the role of psychological flexibility and engaged living. Aging & Mental Health. 2020;24(12):2117-24. [PMID: 31591900] [DOI]
20. Arslan G, Allen K-A. Exploring the association between coronavirus stress, meaning in life, psychological flexibility, and subjective well-being Psychology, Health & Medicine. 2022;27(4):803-14. [PMID: 33487048] [DOI]
21. Ben-Ari A, Aloni R, Ben-David S, Benarroch F, Margalit D. Parental Psychological Flexibility as a Mediating Factor of Post-Traumatic Stress Disorder in Children after Hospitalization or Surgery. International Journal of Environmental Research and Public Health. 2021;18(21):11699. [PMID: 34770210] [PMCID: PMC8582780] [DOI]
22. Davis AK, Barrett FS, Griffiths RR. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. Journal of Contextual Behavioral Science. 2020;15:39-45. [PMID: 32864325] [PMCID: PMC7451132] [DOI]
23. Wang X, Ma H, Li X, Heianza Y, Manson JE, Franco OH, Qi L. Association of Cardiovascular Health With Life Expectancy Free of Cardiovascular Disease, Diabetes, Cancer, and Dementia in UK Adults. JAMA Internal Medicine. 2023;183(4):340-9. [PMID: 36848126] [PMCID: PMC9972243] [DOI]
24. Ma H, Wang X, Xue Q, Li X, Liang Z, Heianza Y, et al. Cardiovascular Health and Life Expectancy Among Adults in the United States. Circulation. 2023;147(15):1137-46. [PMID: 37036905] [PMCID: PMC10165723] [DOI]
25. Tian Q, Chen S, Zhang J, Li C, Wu S, Wang Y, Wang Y. Ideal cardiovascular health metrics and life expectancy free of cardiovascular diseases: a prospective cohort study. EPMA Journal. 2023;14(2):185-99. [PMID: 37275553] [DOI]
26. Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ. 2020;368:l6669. [PMID: 31915124] [PMCID: PMC7190036] [DOI]
27. Nicolescu S, Secară E-C, Jiboc NM, Băban A. Oncovox: A randomised controlled trial of a web-based acceptance and commitment therapy for breast cancer patients. Journal of Contextual Behavioral Science. 2024;32:100729. [DOI]
28. Levin ME, Krafft J, Twohig MP. An Overview of Research on Acceptance and Commitment Therapy. Psychiatric Clinics of North America. 2024. [DOI]
29. Gallego A, Serrat M, Royuela-Colomer E, Sanabria-Mazo JP, Borràs X, Esteve M, et al. Study protocol for a three-arm randomized controlled trial investigating the effectiveness, cost-utility, and physiological effects of a fully self-guided digital Acceptance and Commitment Therapy for Spanish patients with fibromyalgia. DIGITAL HEALTH. 2024;10:20552076241239177. [PMID: 38550263] [PMCID: PMC10976514] [DOI]
30. Sloshower J, Guss J, Krause R, Wallace RM, Williams MT, Reed S, Skinta MD. Psilocybin-assisted therapy of major depressive disorder using Acceptance and Commitment Therapy as a therapeutic frame. Journal of Contextual Behavioral Science. 2020;15:12-9. [DOI]
31. Rostami M, Fatollahzadeh N, Saadati N, Rostami M. The effectiveness of acceptance and commitment training on improving the quality of life and self-compassion of the mothers of educable disabled children. Journal of Psychological Studies. 2016;12(3):103-22.
32. Wersebe H, Lieb R, Meyer AH, Hofer P, Gloster AT. The link between stress, well-being, and psychological flexibility during an Acceptance and Commitment Therapy self-help intervention. International Journal of Clinical and Health Psychology. 2018;18(1):60-8. [PMID: 30487911] [PMCID: PMC6220909] [DOI]
33. Iturbe I, Echeburúa E, Maiz E. The effectiveness of acceptance and commitment therapy upon weight management and psychological well-being of adults with overweight or obesity: A systematic review. Clinical Psychology & Psychotherapy. 2022;29(3):837-56. [PMID: 34802174] [DOI]
34. Mogadam N, Amraae R, Asadi F, Amani O. The Efficacy of Acceptance and Commitment Therapy (ACT) on Hope and Psychological Well-being in Women with Breast Cancer under Chemotherapy. Journal of Nursing Education. 2018;6(5):1-8.
35. Graham CD, Gouick J, Krahé C, Gillanders D. A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clinical Psychology Review. 2016;46:46-58. [PMID: 27176925] [DOI]
36. Donisi V, Poli S, Berti L, Gobbin F, Giusto G, Capurso M, et al. Combining acceptance and commitment therapy with adventure therapy to face vulnerability: Examples and insights from a sailing experience. Journal of Contextual Behavioral Science. 2024:100759. [DOI]
37. Mohamadinikoo Z, Tamannaeifar M. Structural Model of psychological Well-being based on Basic Psychological Needs and Mindfulness With the Mediating role of Problematic internet Use in adolescents. Rooyesh-e-Ravanshenasi Journal(RRJ). 2024;13(1):19-28.
38. Golparvar M, Parsakia K. Building Resilience: Psychological Approaches to Prevent Burnout in Health Professionals. KMAN Counseling & Psychology Nexus. 2023;1(1):159-66. [DOI]
39. Hayes SC. Acceptance & Commitment Therapy (ACT) 2020 [Available from: https://contextualscience.org/.
40. Bakhshandeh Larimi N, Zebardast A, Rezaei S. The effectiveness of acceptance and commitment therapy on cognitive flexibility, rumination, and distress tolerance in persons with Migraine headache. Shenakht Journal of Psychology and Psychiatry. 2021;8(2):74-87. [DOI]
41. Fauth EB, Novak JR, Levin ME. Outcomes from a pilot online Acceptance and Commitment Therapy program for dementia family caregivers. Aging & Mental Health. 2022;26(8):1620-9. [PMID: 34233133] [DOI]
42. Mohammadi S, Fattahi A, Jaberghaderi N, Kheirabadi Z, Bakhtiari M. The effectiveness of acceptance and commitment therapy (ACT) on sleep quality and quality of life of patients with cardiovascular problems. Shenakht Journal of Psychology and Psychiatry. 2022;9(3):85-96. [DOI]
43. Solimanpour M, Pirkhaefi A, Zahrakar k. Comparison of the efficacy of acceptance and commitment therapy (ACT) and compassion-focused therapy (CFT) on quality of life in patients with vitiligo. Journal of Psychological Science. 2022;21(113):987-1004. [DOI]
Downloads
Additional Files
Published
License
Copyright (c) 2024 Atena Naseri (Author); Mahdieh Rahmanian (Corresponding Author); Amin Rafieipour (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.