Investigating the Levels of Lymphocytes, White Blood Cells, and Platelets in Middle-Aged Active and Inactive Individuals Infected with COVID-19 Hospitalized at Vali-e-Asr Hospital in Birjand City
Keywords:
COVID-19, physical activity, lymphocytes, white blood cells, platelets, middle-aged, hematological parametersAbstract
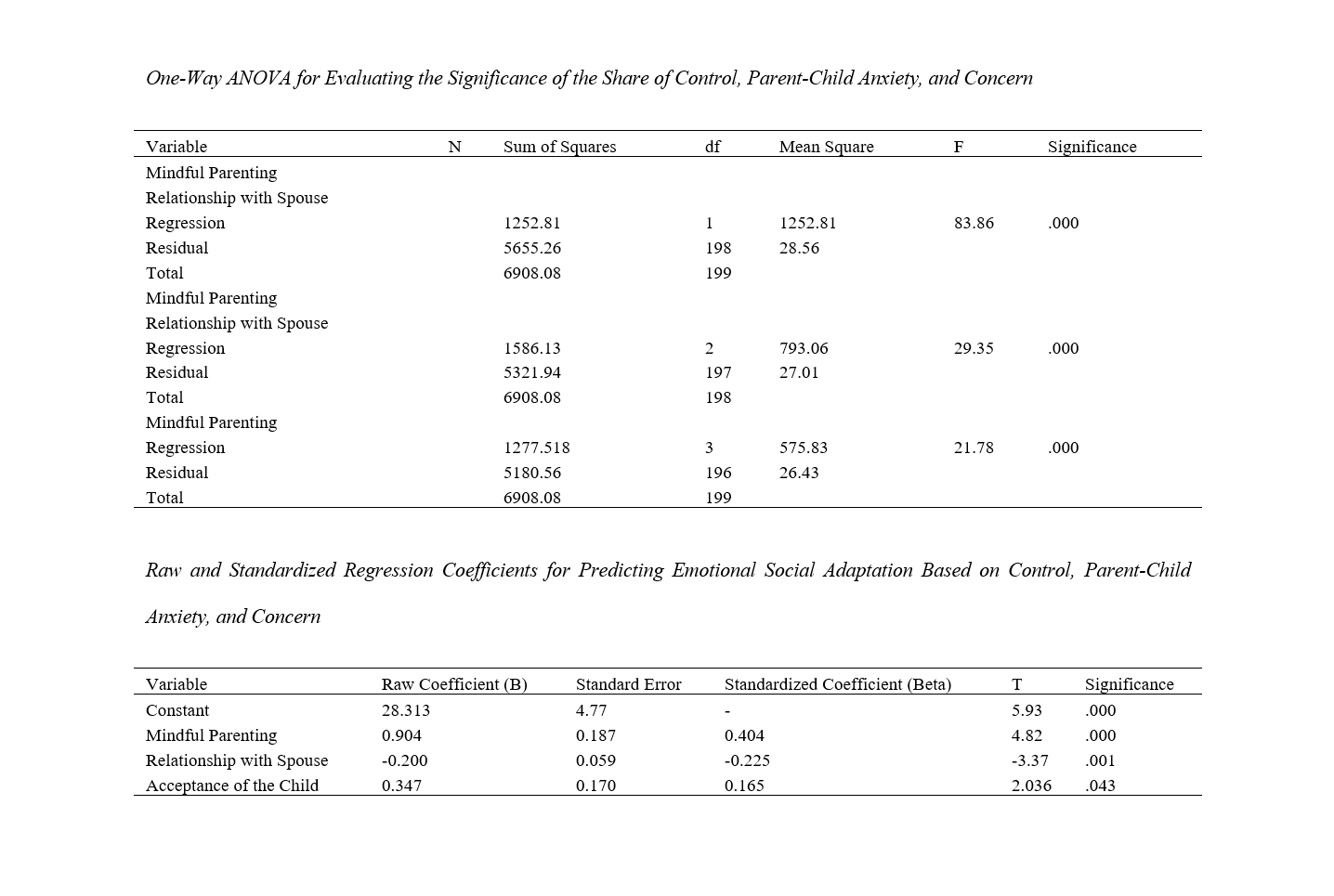
This study aimed to evaluate the impact of physical activity on hematological parameters, specifically lymphocytes, white blood cells (WBC), and platelets, among middle-aged individuals infected with COVID-19. The objective was to determine whether physical activity levels are associated with differences in these key immune markers. A cross-sectional study design was utilized, encompassing 144 middle-aged (35-60 years) COVID-19 patients hospitalized at Vali-e-Asr Hospital in Birjand city. Participants were categorized into active and inactive groups based on their self-reported physical activity levels. Hematological parameters, including lymphocyte, WBC, and platelet counts, were measured and analyzed. Statistical analysis included descriptive statistics and the Mann-Whitney U test to compare differences between groups. The study revealed significant differences in hematological parameters between physically active and inactive patients. Active individuals exhibited higher mean lymphocyte counts (2.48 ± 0.33 vs. 2.47 ± 0.34, p>0.05), WBC (6.55 ± 1.25 vs. 6.52 ± 1.24, p>0.05), and platelet counts (250.50 ± 45.00 vs. 249.95 ± 44.95, p>0.05) compared to their inactive counterparts, although the differences were not statistically significant, suggesting a potential modulatory effect of physical activity on immune markers in COVID-19 patients. Physical activity may have a beneficial impact on the immune response of middle-aged COVID-19 patients, as indicated by the differences in key hematological parameters between active and inactive individuals. However, the observed differences were not statistically significant, underscoring the need for further research to explore the relationship between physical activity and immune function in the context of COVID-19. Future studies should aim to employ longitudinal designs, objective measures of physical activity, and broader population samples to validate and extend these findings.
Downloads
References
1. Al-Atawi AA, Khan F, Kim CG. Application and Challenges of IoT Healthcare System in COVID-19. Sensors. 2022. [PMID: 36236404] [PMCID: PMC9571605] [DOI]
2. Zhang Y, Zhang H, Ma X, Di Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. International journal of environmental research and public health. 2020;17(10):3722. [PMID: 32466163] [PMCID: PMC7277113] [DOI]
3. Dai W, Zhong A, Qiao Q, Wu J, Li W, Wu Q, et al. Characteristics of Lymphocyte Subset Alterations in COVID-19 Patients With Different Levels of Disease Severity. Virology Journal. 2022. [PMID: 36403042] [PMCID: PMC9675966] [DOI]
4. Wang F, Nie J, Wang H, Zhao Q, Xiong Y, Deng L, et al. Characteristics of Peripheral Lymphocyte Subset Alteration in COVID-19 Pneumonia. The Journal of Infectious Diseases. 2020. [PMID: 32227123] [PMCID: PMC7184346] [DOI]
5. Chu M. The Correlation of Lymphocytes With Disease Progression of COVID-19. Medicine. 2023. [PMID: 38050270] [PMCID: PMC10695541] [DOI]
6. Alnor A, Sandberg MB, Toftanes BE, Vinholt PJ. Platelet Parameters and Leukocyte Morphology Is Altered in COVID-19 Patients Compared to Non-Covid-19 Patients With Similar Symptomatology. Scandinavian Journal of Clinical and Laboratory Investigation. 2021. [PMID: 33685285] [DOI]
7. Ignatyev O, Panyita O, L PT, S KP. Haematological Changes in Sailors Who Had COVID-19. International Maritime Health. 2022. [PMID: 36583404] [DOI]
8. Habib MB, Abdelghani MS, Elyas A, Ashour AA, Altermanini M, Imran S, Arabi AR. Acute Thrombotic Occlusion Involving Three Coronary Arteries. A Unique Association With COVID‐19 Pneumonia. Clinical Case Reports. 2023. [PMID: 37593346] [PMCID: PMC10427750] [DOI]
9. Galluzzo V, Zazzara MB, Ciciarello F, Tosato M, Martone AM, Pais C, et al. Inadequate Physical Activity Is Associated With Worse Physical Function in a Sample of COVID-19 Survivors With Post-Acute Symptoms. Journal of Clinical Medicine. 2023. [PMID: 37048602] [PMCID: PMC10095156] [DOI]
10. KoÇ İ, Özmen SÜ. Eosinophil Levels, Neutrophil-Lymphocyte Ratio, and Platelet-Lymphocyte Ratio in the Cytokine Storm Period of Patients With COVID-19. International Journal of Clinical Practice. 2022. [PMID: 35950101] [PMCID: PMC9346569] [DOI]
11. Liu K, Chen Y, Lin R, Han K. Clinical Features of COVID-19 in Elderly Patients: A Comparison With Young and Middle-Aged Patients. Journal of Infection. 2020. [PMID: 32171866] [PMCID: PMC7102640] [DOI]
12. Demombynes G, Walque Dd, Gubbins P, Urdinola P, Veillard J. Are COVID-19 Age-Mortality Curves for 2020 Flatter in Developing Countries? Evidence From a Cross-Sectional Observational Study of Population-Level Official Death Counts and Excess Deaths Estimates. BMJ Open. 2022. [DOI]
13. Nieman DC, Pedersen BK. Exercise and Immune Function. Sports Medicine. 1999. [DOI]
14. Wei T, Li J, Cheng Z, Jiang L, Zhang J, Wang H, Zhou L. Hematological Characteristics of COVID‐19 Patients With Fever Infected by the Omicron Variant in Shanghai: A Retrospective Cohort Study in China. Journal of Clinical Laboratory Analysis. 2022. [PMID: 36525342] [PMCID: PMC9833982] [DOI]
15. Cheung CL, Ho S-C, Krishnamoorthy S, Li GH. COVID‐19 and Platelet Traits: A Bidirectional Mendelian Randomization Study. Journal of Medical Virology. 2022. [PMID: 35676178] [PMCID: PMC9348324] [DOI]
16. Rayes J, Bourne JH, Brill A, Watson SP. The Dual Role of Platelet‐innate Immune Cell Interactions in Thrombo‐inflammation. Research and Practice in Thrombosis and Haemostasis. 2020. [PMID: 33749995] [PMCID: PMC8251141] [DOI]
17. Rolla R, Puricelli C, Bertoni A, Boggio E, Gigliotti CL, Chiocchetti A, et al. Platelets: "Multiple Choice" Effectors in the Immune Response and Their Implication in COVID‐19 Thromboinflammatory Process. International Journal of Laboratory Hematology. 2021. [PMID: 33725341] [PMCID: PMC8053180] [DOI]
18. Sun Y, Zhou J, Ye K. White Blood Cells and Severe COVID-19: A Mendelian Randomization Study. Journal of Personalized Medicine. 2021. [DOI]
Downloads
Additional Files
Published
License

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.